The Connection between Plaque Psoriasis and Joint Pain
Understanding Plaque Psoriasis and its Effects
As a person who has dealt with plaque psoriasis for years, I can attest to the fact that it is much more than just a skin condition. The red, scaly patches that are the hallmark of this chronic autoimmune disease are often accompanied by a host of other symptoms. One of these that we often don't talk about enough is joint pain.
Plaque psoriasis typically presents with inflamed, red, scaly patches on the skin. It's a condition that affects approximately 2-3% of the global population. However, what many people don't realize is that for a significant number of psoriasis sufferers, joint pain is a serious concern.
The Link Between Plaque Psoriasis and Joint Pain
Joint pain in psoriasis patients is not a coincidence. There is a very real and scientifically documented link between the two. This is because psoriasis is an autoimmune disease, which means that it's caused by the immune system mistakenly attacking healthy cells in the body. In the case of plaque psoriasis, this attack primarily affects the skin. But for some people, it also hits the joints.
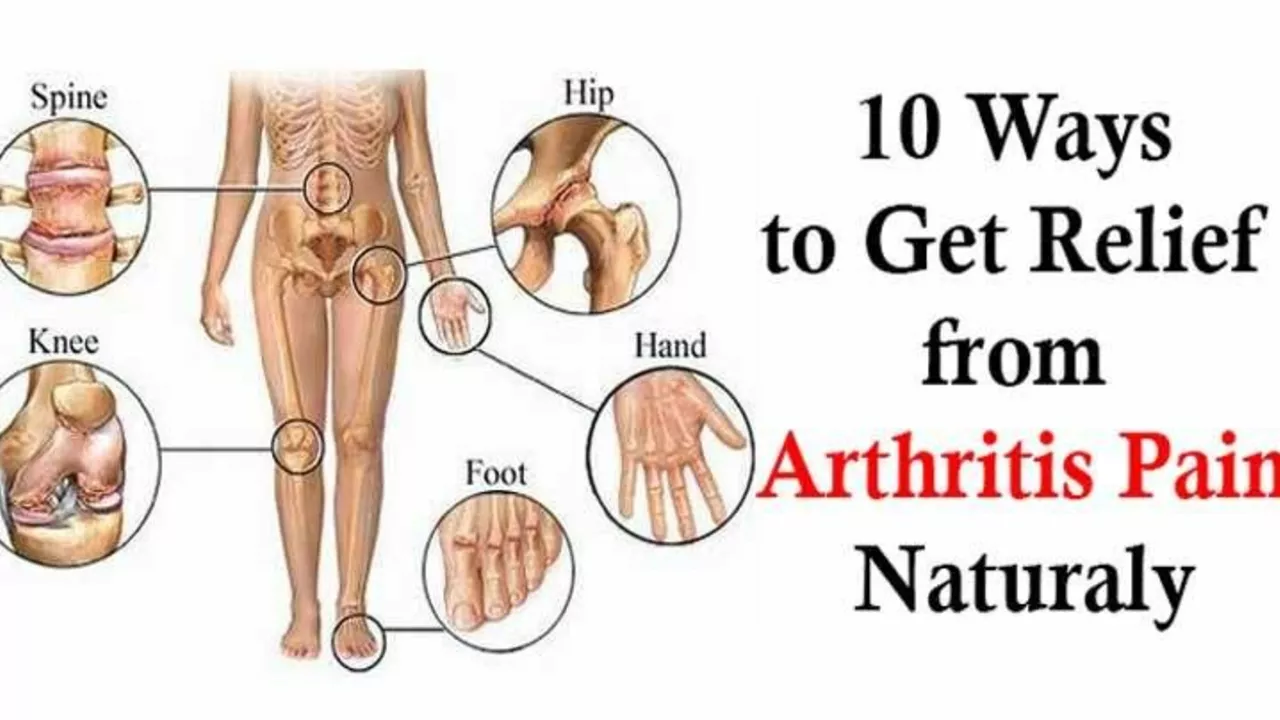
The joint condition associated with psoriasis is known as psoriatic arthritis. Up to 30% of people with psoriasis will develop this form of arthritis at some point in their life. It can cause pain, stiffness, and swelling in any joint in the body, and in severe cases, it can lead to irreversible joint damage.
Recognizing Psoriatic Arthritis
One of the challenges with psoriatic arthritis is that its symptoms can be quite varied. Some people experience mild joint pain that comes and goes. Others may have severe joint pain that lasts for weeks or months at a time.
Common symptoms of psoriatic arthritis include pain and swelling in one or more joints, often the fingers and toes, lower back pain, fatigue, and reduced range of motion. These symptoms can significantly impact a person's quality of life, making it difficult to perform everyday tasks and activities.
Treating Psoriasis and Joint Pain
The good news is that there are treatments available for both plaque psoriasis and psoriatic arthritis. These can help to manage symptoms and slow down the progression of the disease.
Treatments for plaque psoriasis typically involve topical creams, light therapy, and systemic medications. For psoriatic arthritis, nonsteroidal anti-inflammatory drugs (NSAIDs), disease-modifying antirheumatic drugs (DMARDs), and biologics are commonly used. It's also important to maintain a healthy lifestyle, including regular exercise and a balanced diet, to help manage symptoms.
Living with Plaque Psoriasis and Joint Pain
Living with plaque psoriasis and joint pain can be challenging, but it's important to remember that you're not alone. There are support groups and resources available to help you navigate this journey. It's also crucial to work closely with your healthcare provider to find a treatment plan that works for you.
Remember, plaque psoriasis and joint pain don't have to define you. With the right treatment and support, you can manage your symptoms and lead a fulfilling life. Make sure to reach out to your healthcare provider if you're experiencing joint pain along with your plaque psoriasis. Early diagnosis and treatment can make a significant difference in managing this condition.






Comments
Miah O'Malley
July 21, 2023 AT 17:20Living with psoriasis and joint pain whispers a deeper lesson about the fragility and resilience of the human body. When skin erupts like a storm, the joints often echo the same turmoil, reminding us that inflammation is not merely a surface phenomenon. The mind learns to negotiate with discomfort, turning each flare into a meditation on impermanence. By observing the pattern of symptoms, we can cultivate a compassionate awareness that transcends the medical jargon. In this way, our bodies become teachers rather than adversaries.
Bradley Allan
July 26, 2023 AT 08:27Wow!!! Who would have thought that a simple rash could hide a ticking time‑bomb of joint devastation??? The audacity of the immune system to betray its own host is nothing short of theatrical!!! We are forced to juggle creams, pills, and endless doctor visits-only to discover that the real battle rages beneath the skin!!!
Kyle Garrity
July 29, 2023 AT 19:47Reading your reflections really hits home-I've been wrestling with the same sting in my knees for years, and your words give me a sense of calm amidst the flare‑ups. Knowing I'm not alone makes the daily grind a little easier to bear.
brandon lee
August 1, 2023 AT 03:20Psoriasis is a beast, but you can still enjoy a good laugh.
Joshua Pisueña
August 4, 2023 AT 00:47Stay active and keep moving forward even when the joints protest; small daily walks can make a huge difference over time.
Ralph Barcelos de Azevedo
August 5, 2023 AT 18:27It is incumbent upon us to demand comprehensive care from our healthcare system rather than settle for superficial skin treatments; the moral obligation to address psoriatic arthritis is undeniable.
Peter Rupar
August 9, 2023 AT 05:47Yo, stop ignoring the joint pain like it's just a lil ache-this stuff can wreck your life if you don't take it seriouusly!!!
Nikita Shue
August 10, 2023 AT 09:33Exactly, bro-listen to your body, get a rheumatologist, and don't let the fear hold you back!
Heather McCormick
August 12, 2023 AT 17:07Oh great, another post telling us to "stay positive" while the pharma giants keep cashing in on our misery. How original.
Robert Urban
August 14, 2023 AT 02:27While it's true that corporate interests cloud the conversation, we still have effective therapies that can improve quality of life-let's focus on what works.
Stephen Wunker
August 16, 2023 AT 04:27One could argue that labeling psoriasis as merely an autoimmune glitch ignores the existential narrative our bodies write: a rebellion against conformity.
Jhoan Farrell
August 17, 2023 AT 02:40That perspective is fascinating 🤔-thanks for sharing!
Jill Raney
August 18, 2023 AT 20:20The mainstream narrative is deliberately diluted to keep us compliant; only the enlightened see the hidden geopolitical implications 😒.
bill bevilacqua
August 19, 2023 AT 15:47Honestly, who cares about all that conspiracy stuff-it’s just a health issue, not a political plot!!!
rose rose
August 20, 2023 AT 19:33All the cures are being hidden by the government.
Emmy Segerqvist
August 21, 2023 AT 20:33Seriously, the struggle is real!!! Every morning I wake up, stare at the mirror, and wonder how much longer I can survive this relentless onslaught!!!
Trudy Callahan
August 22, 2023 AT 13:13Perhaps the mirror is merely a cosmic reflection of our internal discord, urging us to reconcile mind, skin, and soul!!!
Grace Baxter
August 24, 2023 AT 20:47When I first heard about the connection between plaque psoriasis and joint pain, I thought it was just another medical footnote, but the reality is far more intricate. The immune system, in its misguided quest, launches attacks that manifest on the skin and then infiltrate the synovial membranes of our joints. This dual assault creates a feedback loop where inflammation fuels more inflammation, making each flare feel like a domino effect. Researchers have identified cytokines-especially TNF‑alpha and IL‑17-as the culprits that amplify both dermatologic and arthritic symptoms. Consequently, therapies targeting these molecules, such as biologics, have revolutionized treatment, offering relief that skin creams alone could never achieve. Yet, access to these advanced medications remains uneven, with insurance hurdles and cost barriers turning hope into frustration for many patients. Moreover, lifestyle factors like diet, stress management, and regular low‑impact exercise play a surprisingly pivotal role in modulating disease activity. A balanced omega‑3 intake, for instance, can dampen inflammatory pathways, while chronic stress reverses any pharmacologic gains. It's also crucial to recognize that early diagnosis of psoriatic arthritis can prevent irreversible joint damage, underscoring the importance of routine screenings for anyone with moderate to severe psoriasis. Dermatologists and rheumatologists must collaborate closely, sharing patient histories to tailor a holistic plan. In practice, this means setting up multidisciplinary clinics where a single visit can address skin lesions, joint assessments, and mental health support. Speaking of mental health, the psychosocial burden of visible skin lesions combined with hidden joint pain often leads to anxiety and depression, which in turn exacerbate inflammation-a vicious cycle that only comprehensive care can break. Patient education, therefore, becomes a cornerstone: teaching individuals to recognize early joint swelling, to advocate for appropriate imaging, and to stay informed about emerging therapies. Finally, community support groups-both online and offline-provide the emotional scaffolding needed when the disease feels isolating. Sharing stories, coping strategies, and triumphs can inspire adherence to treatment plans and foster resilience. In sum, the intersection of plaque psoriasis and joint pain is a complex tapestry woven from immunology, genetics, environment, and lived experience, demanding a nuanced, patient‑centered approach.
Eddie Mark
August 25, 2023 AT 10:40That was a marathon of thoughts-awesome deep dive!