Antibiotic-Related Liver Injury: What You Need to Know About Hepatitis and Cholestasis
Liver Injury Calculator
How to Use This Calculator
This calculator determines the type of antibiotic-related liver injury based on your ALT and ALP lab values using the R-ratio method described in the article.
Result
Your R-ratio is:
Antibiotics save lives. But for some people, they also damage the liver - sometimes without warning. If you’ve ever been prescribed amoxicillin-clavulanate, ciprofloxacin, or piperacillin-tazobactam and later found out your liver enzymes were high, you’re not alone. Antibiotic-related liver injury is more common than most patients and even some doctors realize. In fact, antibiotics cause about 64% of all drug-induced liver injury cases, especially in hospitalized patients. This isn’t rare. It’s routine - and often missed.
How Antibiotics Hurt the Liver
Antibiotics don’t just kill bacteria. They disrupt your body’s balance in ways that can turn toxic. The liver processes almost everything you take - including antibiotics. Some antibiotics get broken down into harmful byproducts that stress liver cells. Others directly interfere with mitochondria, the energy factories inside liver cells. When mitochondria fail, cells start dying. That’s hepatitis.
Then there’s cholestasis. This happens when bile can’t flow properly out of the liver. Antibiotics like amoxicillin-clavulanate are notorious for this. They block the bile salt export pump (BSEP), a key protein that moves bile out of liver cells. When bile backs up, it damages the liver from the inside. You won’t always feel it. Many people only find out through routine blood tests.
The gut plays a bigger role than you think. Antibiotics wipe out good bacteria in your intestines. That lets bad ones take over. These bad bacteria produce toxins that leak into the bloodstream and reach the liver. Studies show that people with lower levels of Faecalibacterium prausnitzii - a beneficial gut bacterium - have over three times the risk of developing liver injury after antibiotics. Your gut health isn’t just about digestion. It’s a shield for your liver.
Hepatitis vs. Cholestasis: The Two Faces of Liver Injury
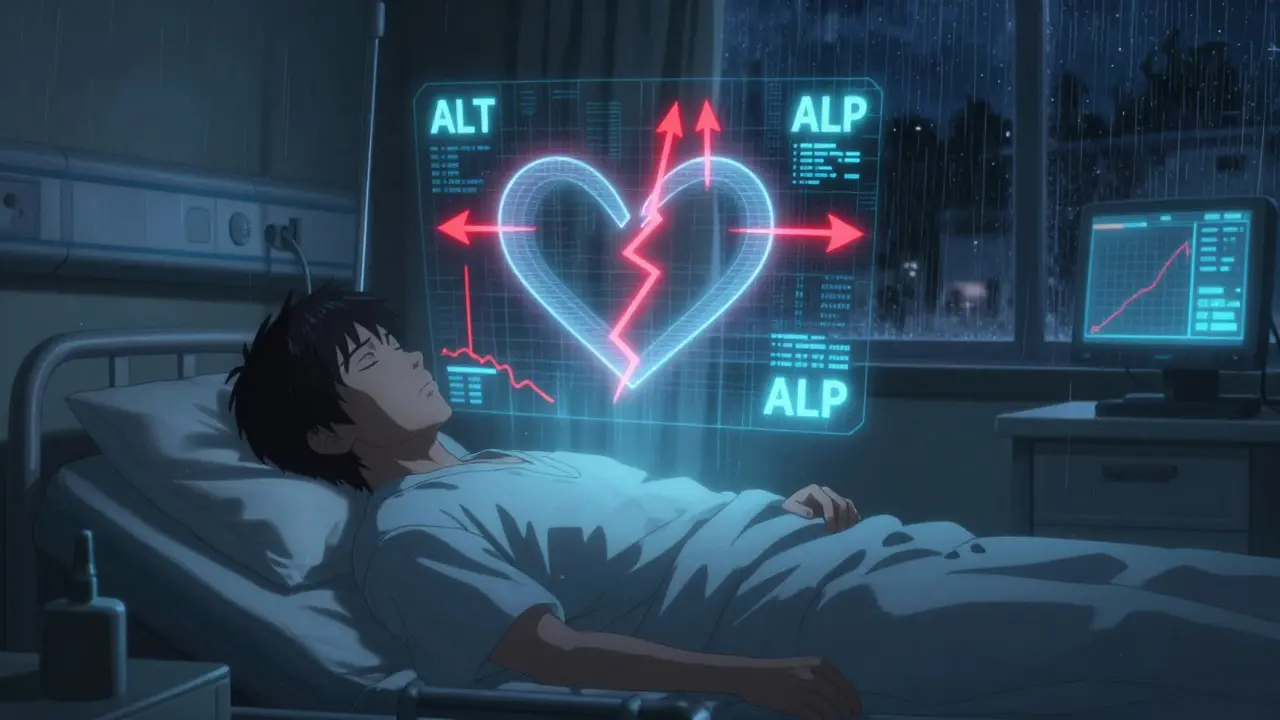
Not all antibiotic liver damage looks the same. Doctors use a simple number - the R-ratio - to tell them what’s happening. It’s calculated by dividing the ratio of your ALT (a liver enzyme) to its normal limit by the ratio of your ALP (another liver enzyme) to its normal limit.
- If R > 5: You have hepatocellular injury - liver cells are dying. ALT is sky-high. This looks like viral hepatitis.
- If R < 2: You have cholestatic injury - bile flow is blocked. ALP and bilirubin are up. You might turn yellow.
- If R is between 2 and 5: It’s mixed. You’re seeing both patterns.
Amoxicillin-clavulanate? Over 70% of cases are cholestatic. Ciprofloxacin and azithromycin? More often mixed. This matters because the symptoms and recovery time differ. Hepatitis can cause fatigue, nausea, and dark urine. Cholestasis often brings itching, pale stools, and jaundice. Some people feel fine - until their bloodwork screams for attention.
Which Antibiotics Are Most Dangerous?
Not all antibiotics carry the same risk. The LiverTox database, maintained by the National Institutes of Health, ranks them by danger level. Here’s what the data shows:
| Antibiotic | Typical Injury Pattern | Incidence per 100,000 Prescriptions | Risk Category (LiverTox) |
|---|---|---|---|
| Amoxicillin-clavulanate | Cholestatic | 15-20 | High (8-10) |
| Piperacillin-tazobactam (TZP) | Mixed | Up to 28.7% in ICU | High (8-10) |
| Ciprofloxacin | Mixed | 1-3 | Moderate (5-7) |
| Azithromycin | Mixed | 1-2 | Moderate (5-7) |
| Nitrofurantoin | Hepatocellular | 1-3 | Moderate (5-7) |
| Trimethoprim-sulfamethoxazole | Hepatocellular | 1-3 | Moderate (5-7) |
| Meropenem | Hepatocellular | 12.3% in ICU | Moderate (5-7) |
Amoxicillin-clavulanate is the biggest offender. It’s one of the most commonly prescribed antibiotics - and one of the most likely to hurt the liver. Piperacillin-tazobactam is even riskier in hospitals. One study found that nearly 3 in 10 ICU patients on this drug developed liver injury. And if you’re male and on meropenem? Your risk is 2.4 times higher than a woman’s.
When Does It Happen?
Timing matters. If you start an antibiotic and feel fine for three weeks, don’t assume you’re safe. Amoxicillin-clavulanate often causes injury 1 to 6 weeks after starting. Fluoroquinolones like ciprofloxacin can hit faster - within days. The longer you’re on antibiotics, the higher the risk. Taking them for 7 days or more increases your chance of liver injury by over three times. That’s not a small risk. It’s a red flag.
And it’s not just the drug. Your health matters too. If you’re sick with sepsis, your liver is already under stress. Antibiotics can push it over the edge. Studies show sepsis makes liver injury 1.8 times more likely during antibiotic treatment. People with existing liver disease, older adults, and those on multiple medications are also at higher risk.
How Do Doctors Spot It?
There’s no single test. No scan shows it. No symptom is unique. The diagnosis is a process of elimination. Doctors look at your blood work, your timeline, and your meds. They rule out viruses, alcohol, fatty liver, and other causes.
Standard thresholds help:
- ALT > 5× upper limit of normal → Hepatocellular injury
- ALP > 2× upper limit of normal → Cholestatic injury
- ALT > 3× + bilirubin > 2× → Mixed injury
But here’s the catch: many patients have no symptoms. They feel fine. Their ALT is just slightly up. Should they stop the antibiotic? Maybe. Maybe not. That’s why guidelines say: stop if ALT exceeds 5× ULN and you have symptoms. But in real life, many doctors stop earlier - especially if the drug is high-risk and alternatives exist.
Monitoring is key. For high-risk antibiotics, baseline liver tests before starting are recommended. Then, repeat tests after 1-2 weeks. If you’re on antibiotics for more than 7 days - especially in the hospital - weekly checks are standard. Many hospitals now track this automatically.
What Happens After You Stop?
Good news: in most cases, the liver heals. Once you stop the antibiotic, enzymes usually start dropping within days. Full recovery takes weeks to months. Most people bounce back completely.
But not everyone. A small number develop lasting damage. Rarely, it leads to acute liver failure. That’s why early detection matters. If you’re jaundiced, itchy, or have dark urine after antibiotics - don’t wait. Get checked.
There’s no antidote. No pill to reverse it. Supportive care is all there is: rest, hydration, avoiding alcohol and other liver stressors. Some doctors try ursodeoxycholic acid for cholestasis, but evidence is weak. The best treatment? Stopping the drug.
What’s Changing in 2026?
Research is moving fast. Scientists now know your genes matter. Certain HLA variants - your immune system’s ID tags - make you more likely to react badly to specific antibiotics. If you have HLA-B*57:01, you’re at higher risk for amoxicillin-clavulanate injury. That’s not routine testing yet - but it’s coming.
One of the most exciting areas is the gut microbiome. Companies are developing stool tests to predict who’s at risk before they even start antibiotics. If your microbiome looks weak - low diversity, low F. prausnitzii - you might avoid high-risk drugs or get a probiotic alongside your prescription.
Clinical trials are testing probiotics to prevent liver injury. Early results are promising. If they work, we could soon be giving patients a daily probiotic along with their antibiotics - not just to prevent diarrhea, but to protect the liver.
Regulators are paying attention. The FDA and EMA now require stronger liver safety data for new antibiotics. Drug companies are more cautious. Some promising antibiotics have been dropped because they caused liver damage in early trials.
What Should You Do?
If you’re prescribed an antibiotic:
- Ask: Is this the best choice for my infection? Are there lower-risk options?
- Ask: Should I get a liver test before starting?
- Ask: Should I get tested again after 1-2 weeks?
- Watch for symptoms: yellow skin, dark urine, itching, nausea, fatigue.
- Don’t ignore blood test results - even if you feel fine.
- If you’re on antibiotics for more than 7 days, make sure your doctor is tracking your liver enzymes.
If you’ve had liver injury before - especially from antibiotics - keep a list of the drugs that caused it. Tell every doctor you see. Avoid those drugs in the future. Your liver remembers.
Antibiotics are essential. But they’re not harmless. Understanding the risks - and asking the right questions - can keep your liver safe while you fight infection.


Comments
vivek kumar
January 16, 2026 AT 16:38Amoxicillin-clavulanate is the silent killer in every antibiotic prescription. I got mine after a sinus infection, felt fine for three weeks, then woke up yellow. No pain, no nausea, just a routine blood test that nearly ended my life. Doctors act like it's rare. It's not. It's the #1 cause of drug-induced liver failure in my hospital. Why aren't we screening everyone? Why are we still prescribing it like it's Advil?
Riya Katyal
January 18, 2026 AT 14:29Oh wow, so antibiotics aren't magic fairy dust? Who knew? 🙃 Maybe if people stopped demanding them for every sniffle, we wouldn't be poisoning our livers. But hey, I'm sure your 'gut health' TikTok guru will sell you a $40 probiotic to fix it.
Isabella Reid
January 20, 2026 AT 14:23I'm a nurse in a rural ER, and this post is spot on. We see this all the time - patients come in with jaundice, and the first thing they say is, 'I just took that antibiotic for my tooth infection.' No symptoms. No warning. Just elevated enzymes. We've started doing baseline LFTs on anyone over 50 getting amoxicillin-clavulanate. It's not perfect, but it's better than waiting for them to turn into a human lemon.
Jody Fahrenkrug
January 21, 2026 AT 21:49My mom had this after a UTI. She was fine until her skin turned the color of old parchment. Took 4 months for her enzymes to normalize. We never knew antibiotics could do that. Now I ask every doctor: 'What's the liver risk?' They look at me like I'm crazy. But I'd rather be the weird one than the dead one.
Kasey Summerer
January 23, 2026 AT 14:50So let me get this straight - we're giving people antibiotics that can fry their liver, and the only 'treatment' is to stop taking them? 😂 I mean, what's next? 'Hey, your car's on fire - just turn off the ignition.' Also, if you're on azithromycin and itching like a dog with fleas... stop. Just stop. 🤦♂️
Allen Davidson
January 24, 2026 AT 09:52Stop blaming the drugs. Blame the system. We're overprescribing antibiotics because doctors are rushed, patients demand them, and insurance won't cover better tests. This isn't about individual choices - it's about a broken healthcare model. If you want to prevent this, push for better access to rapid diagnostics. Not just 'ask your doctor.' That's not a solution. It's a cop-out.
john Mccoskey
January 25, 2026 AT 21:39Let’s be brutally honest: the liver is not a sacred temple. It’s a biological filter - a glorified garbage disposal. We treat it like it’s fragile porcelain when in reality, it’s been processing ethanol, acetaminophen, NSAIDs, and now antibiotics since the dawn of civilization. The real tragedy isn’t antibiotic-induced cholestasis - it’s that we’ve built a medical culture that treats every side effect like a cosmic betrayal. If you can’t tolerate a drug’s metabolic burden, don’t take it. Simple. No need for HLA typing or microbiome tests. Just use your brain. And if your liver fails? Well, evolution doesn’t care about your prescription.
Travis Craw
January 27, 2026 AT 05:01my doc gave me cipro for a UTI and i was fine till i started itching like crazy. i thought it was a rash. turns out it was cholestasis. i didn't even know what that word meant. now i check my labs after every antibiotic. kinda paranoid but hey, better safe than sorry right?
brooke wright
January 29, 2026 AT 03:36Wait - so you’re telling me that the same antibiotics we’re giving kids for ear infections might be quietly wrecking their livers? And we don’t even test them? And the FDA just lets this happen? I’m not even mad. I’m just… done. This is how people die quietly. No one talks about it. No one warns you. Just… enzymes go up. And then? Silence.
Nick Cole
January 30, 2026 AT 18:20I’ve seen patients bounce back from this. It’s not a death sentence. But it’s not something to shrug off either. If you’re on an antibiotic for more than 7 days, get your liver checked. Period. I’m not a doctor, but I’ve sat with too many people who thought they were fine until they weren’t. Don’t be one of them.
Henry Ip
February 1, 2026 AT 10:41Love this breakdown. The R-ratio is everything. I always tell people: if your ALT is high and you're itchy, stop the drug. No waiting. No 'let's wait and see.' Your liver doesn't negotiate. And if you're on TZP in the ICU? Ask for daily LFTs. No shame in being loud about your health. You're worth it.
waneta rozwan
February 3, 2026 AT 08:22They don't want you to know this. Big Pharma doesn't want you to know that the antibiotics they're pushing are quietly killing people. They'll bury the data, silence the studies, and call you a 'conspiracy theorist' if you speak up. But I've seen it. My cousin died from amoxicillin-clavulanate. They called it 'idiopathic hepatitis.' It was murder by prescription.
swarnima singh
February 4, 2026 AT 20:06you think this is bad? wait till you find out how many people get liver damage from probiotics. no one talks about that. your 'good bacteria' are just as dangerous. the whole thing is a scam. your gut is fine. your liver is fine. you just need to stop worrying. stop taking so many pills. just live. breathe. be. the body knows what to do. you just need to shut up and let it.
kanchan tiwari
February 6, 2026 AT 12:42THEY’RE PUTTING TOXINS IN OUR MEDICINE ON PURPOSE. IT’S A CONTROL TACTIC. THE GOVERNMENT AND BIG PHARMA WANT YOU WEAK. THEY WANT YOU DEPENDENT ON DOCTORS AND LAB TESTS. THEY DON’T WANT YOU HEALTHY. THEY WANT YOU IN THE SYSTEM. THAT’S WHY THEY DON’T WARN YOU. THAT’S WHY THEY DON’T TEST YOU. THEY WANT YOU TO THINK YOU’RE FINE UNTIL YOU’RE NOT. WAKE UP.
Bobbi-Marie Nova
February 7, 2026 AT 08:36Okay but imagine if we just gave everyone a probiotic with their antibiotic. Like, not just for tummy issues - for liver protection too. It’s so simple. Why aren’t we doing this already? I’d take a pill that saves my liver over another antibiotic any day. Let’s make this a thing.