Antidepressant Use in Pregnancy: What You Need to Know About Safety and Side Effects
Antidepressant Safety Calculator
Understanding Pregnancy and Depression Risks
This calculator compares the relative risks of untreated depression versus taking antidepressants during pregnancy using evidence from major studies.
Data shows that untreated depression poses greater risks to both mother and baby than most antidepressants. The most recommended medication for pregnancy is sertraline (Zoloft), which has the best safety profile.
Untreated Depression
Higher Risk
40%+ increase in preterm birth
30%+ increase in low birth weight
25% increase in preeclampsia
50% less likely to attend prenatal visits
Higher risk of suicide
Antidepressant Use
Moderate Risk
Key Takeaways
Untreated depression poses far greater risks to both mother and baby than most antidepressants.
If you're considering changing your medication or starting treatment, talk to both your OB-GYN and psychiatrist.
Depression During Pregnancy Is Real - and Dangerous
One in seven pregnant people in the U.S. experiences depression. That’s not rare. It’s common. And yet, many still avoid taking antidepressants because they’re scared of harming the baby. The truth? Untreated depression poses a far greater risk to both mother and child than most medications do.
When depression goes unmanaged during pregnancy, the chances of preterm birth go up by 40%. Low birth weight becomes 30% more likely. Preeclampsia risk rises by 25%. The mother is half as likely to show up for prenatal visits. And in the worst cases, depression leads to suicide - the leading cause of pregnancy-related death in the U.S. between 2017 and 2019, according to the CDC.
So when someone asks, “Is it safe to take antidepressants while pregnant?”, the real question should be: “Is it safer to take them - or not?”
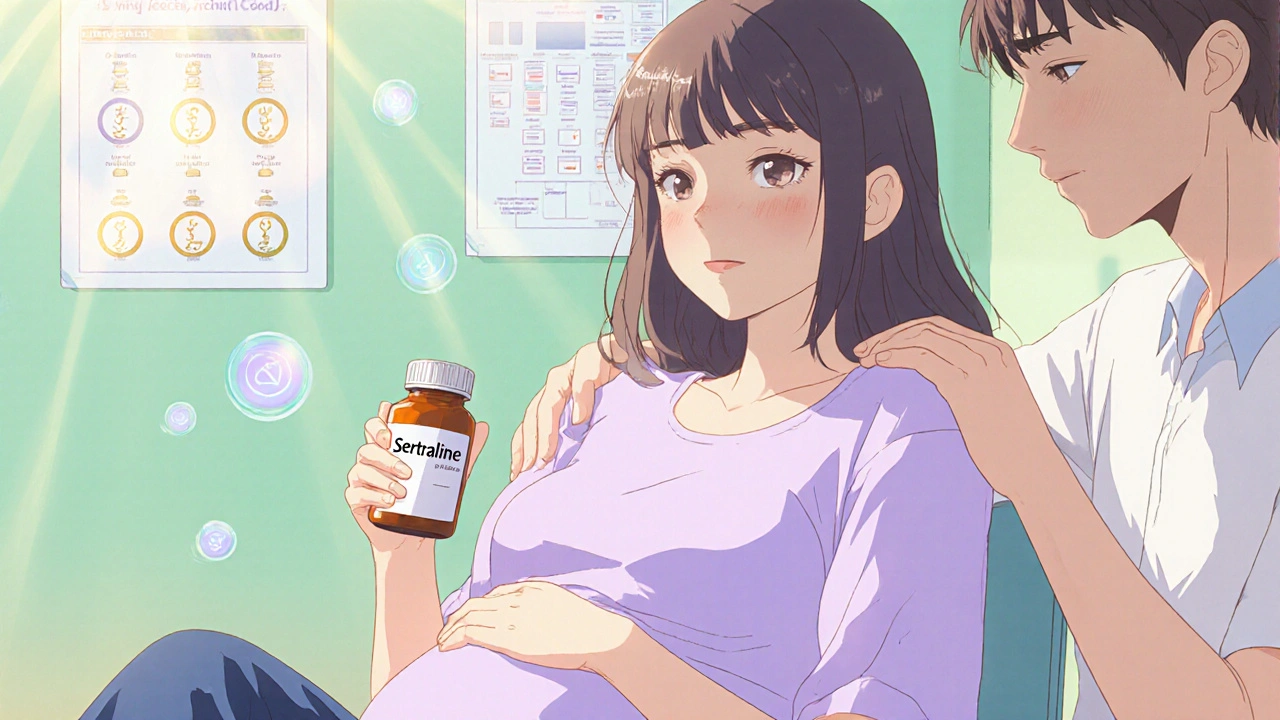
SSRIs Are the First Choice - and Here’s Why
Not all antidepressants are the same. For pregnancy, doctors almost always start with SSRIs - selective serotonin reuptake inhibitors. These include sertraline (Zoloft), citalopram (Celexa), escitalopram (Lexapro), and fluoxetine (Prozac). Among them, sertraline is the most studied and the most recommended.
Why sertraline? Because over 20 years of data show it has the lowest risk profile. It doesn’t cross the placenta as easily as others. It’s less likely to cause side effects in the newborn. And most importantly, large studies tracking millions of pregnancies have found no link between sertraline and major birth defects.
That’s not true for paroxetine (Paxil). It’s an SSRI too - but it’s the exception. Studies show it carries a 1.5 to 2 times higher risk of heart defects in babies. If you’re on paroxetine and planning pregnancy, or just found out you’re pregnant, talk to your doctor about switching. Don’t stop cold turkey - switch under supervision.
What About Birth Defects? The Data Doesn’t Support the Fear
Back in the 2000s, early studies suggested SSRIs might raise the risk of birth defects. But those studies didn’t account for one big thing: the depression itself.
Here’s what the latest science shows: when researchers compared women taking SSRIs to women with depression who didn’t take meds, the difference in birth defect rates vanished. One major 2024 review of 29 studies - covering over 5 million pregnancies - found that the initial signal of higher risk disappeared once they controlled for maternal mental health.
The same goes for major congenital anomalies. A 2018 meta-analysis of 28 high-quality studies showed a tiny increase in risk - but only in women without diagnosed depression. When they looked only at women with confirmed depression, the risk was no different than in women not taking any antidepressants.
In other words: the illness, not the medicine, is often the real culprit.
Neonatal Adaptation Syndrome: A Temporary Issue
Some babies exposed to SSRIs in the last trimester may show signs of fussiness, jitteriness, trouble feeding, or mild breathing issues in the first few days after birth. This is called neonatal adaptation syndrome (NAS), or sometimes PNAS (perinatal adaptation syndrome).
It happens in about 30% of exposed newborns. But here’s the key: it’s temporary. It doesn’t cause lasting harm. Symptoms usually clear up within 10 to 14 days. No long-term developmental issues have been linked to it.
And here’s something else: the risk is highest with fluoxetine, because it sticks around in the body longer. Sertraline and citalopram are less likely to cause this. If you’re near your due date and worried, your doctor can adjust your dose or timing to reduce the chance.
What About Long-Term Development?
Parents often worry: “Will my child be different? Will they have autism? Will they struggle in school?”
The largest study to date - the Norwegian Mother, Father and Child Cohort Study - tracked over 44,000 children up to age five. It compared kids exposed to SSRIs in the womb to those who weren’t. No difference in language skills, motor development, behavior, or autism rates.
Other studies in Canada, Sweden, and the U.S. have reached the same conclusion. There’s no evidence that SSRIs cause autism, ADHD, or learning delays.
What does matter? Genetics. Environment. Parental mental health after birth. A mother who is stable, supported, and emotionally available is far more likely to raise a healthy child - regardless of whether she took medication during pregnancy.
The Big Risk: Stopping Your Medication
Many women stop their antidepressants as soon as they find out they’re pregnant. They think they’re protecting the baby. But here’s what happens next:
- 68% of women who stop their meds experience a full depression relapse.
- Only 26% of women who continue their medication relapse.
That’s not a small difference. That’s more than double the risk.
And it’s not just emotional. Relapse means worse prenatal care, more stress hormones, higher blood pressure, and increased risk of preterm labor. It means you’re less likely to eat well, sleep enough, or get the support you need.
A 2025 study in JAMA Network Open found that nearly half of pregnant women stopped refilling their antidepressant prescriptions - but didn’t start therapy or counseling to make up for it. That’s dangerous. Stopping without a plan is like turning off a fire alarm and hoping the house won’t burn down.
What About Other Antidepressants?
SSRIs are the go-to - but sometimes, doctors use other options.
SNRIs like venlafaxine (Effexor) and duloxetine (Cymbalta) are sometimes used if SSRIs don’t work. They’re considered second-line. The data is more limited, but no major red flags have emerged.
Tricyclic antidepressants like nortriptyline and amitriptyline have been around since the 1970s. They’re older, but still safe in pregnancy. They’re rarely used today unless SSRIs fail - mostly because they cause more side effects like dry mouth, drowsiness, or weight gain.
MAOIs? Avoid them. They’re not recommended during pregnancy because of potential interactions and unclear safety data.
And never, ever switch or stop on your own. Talk to your OB-GYN and your psychiatrist together. They need to coordinate your care.

What’s the Best Approach?
There’s no one-size-fits-all. But here’s what experts agree on:
- If your depression is mild, try therapy first - cognitive behavioral therapy (CBT) works well during pregnancy.
- If your depression is moderate to severe, or you’ve had relapses before, medication is often the safer choice.
- Start with sertraline. It’s the most studied and safest.
- Use the lowest dose that works. You don’t need to be on the highest dose just because you’re pregnant.
- Don’t stop cold turkey. If you need to change meds, do it slowly under medical supervision.
- Keep seeing your doctor. Monitor your mood, your baby’s growth, and any side effects.
Many women find that combining medication with therapy and gentle exercise - like walking or prenatal yoga - gives them the best results. You’re not choosing between meds and mental health. You’re choosing both.
The FDA Panel Controversy: Why the Confusion?
In July 2025, an FDA expert panel raised alarms about SSRIs in pregnancy. The media picked it up. Fear spread. Women called their doctors in panic.
But here’s what the panel didn’t say: they didn’t represent the full scope of evidence. Only one of ten panel members emphasized that SSRIs are critical tools to prevent suicide and severe maternal illness.
ACOG, SMFM, and InfantRisk all responded immediately. They called the panel “alarmingly unbalanced.” They reminded everyone that depression kills more pregnant women than hemorrhage or high blood pressure. They warned that fear-driven decisions could cost lives.
The message from every major medical group is clear: don’t let a single panel shake your trust in the science. The evidence hasn’t changed. SSRIs are safe. Untreated depression is not.
Final Thought: Your Mental Health Matters
Being pregnant doesn’t mean you have to suffer in silence. You don’t have to choose between being a good mom and being well. The best thing you can do for your baby is to be emotionally stable, physically cared for, and mentally supported.
Antidepressants aren’t a magic fix. But for many, they’re the bridge back to life - to sleeping, eating, connecting, and feeling like yourself again. And that’s not just good for you. It’s essential for your child.
Are SSRIs safe during pregnancy?
Yes, most SSRIs are considered safe during pregnancy, especially sertraline and citalopram. Large studies involving millions of pregnancies show no increased risk of major birth defects when compared to pregnant women with depression who aren’t taking medication. The risks from untreated depression - including preterm birth, low birth weight, and maternal suicide - are far greater than the risks from these medications.
Can antidepressants cause autism in babies?
No. Multiple large, long-term studies - including one tracking over 44,000 children up to age five - found no link between SSRI use during pregnancy and autism, ADHD, or developmental delays. The idea that antidepressants cause autism comes from outdated or poorly designed studies that didn’t account for the mother’s mental health condition.
Should I stop taking antidepressants if I’m pregnant?
No - not without talking to your doctor. Stopping abruptly increases your chance of relapse by more than double. About 68% of women who stop their meds during pregnancy experience a return of severe depression. That puts both you and your baby at higher risk. If you need to switch or lower your dose, do it slowly and under medical supervision.
Is paroxetine safe during pregnancy?
No. Paroxetine (Paxil) is linked to a higher risk of heart defects in babies - about 1.5 to 2 times higher than other SSRIs. If you’re taking paroxetine and planning pregnancy or are already pregnant, talk to your doctor about switching to sertraline or citalopram. Don’t stop suddenly - switch gradually under care.
What are the side effects for the baby?
Some babies exposed to SSRIs in the third trimester may have temporary symptoms like jitteriness, fast breathing, or trouble feeding - known as neonatal adaptation syndrome. This happens in about 30% of cases but resolves within 10-14 days. It doesn’t cause long-term harm. Sertraline has the lowest risk of this compared to fluoxetine, which stays in the body longer.
Can I breastfeed while taking antidepressants?
Yes. Sertraline and citalopram are the preferred choices for breastfeeding because very little passes into breast milk. Fluoxetine is less ideal because it builds up over time. Most babies show no side effects. The benefits of breastfeeding - bonding, immunity, nutrition - far outweigh the tiny amount of medication that may pass through.
What if I didn’t know I was pregnant and took antidepressants?
Don’t panic. Many women take antidepressants before realizing they’re pregnant. The risk of birth defects from SSRIs is extremely low - especially if you’re on sertraline or citalopram. Talk to your doctor about switching to a safer option if needed, but don’t stop suddenly. Your mental health matters just as much as your baby’s physical health.
Is therapy enough instead of medication?
For mild depression, yes - cognitive behavioral therapy (CBT) can be very effective during pregnancy. But for moderate to severe depression, or if you’ve had depression before, therapy alone isn’t usually enough. Medication and therapy together give the best outcomes. You don’t have to choose one or the other.





Comments
Yash Hemrajani
November 29, 2025 AT 16:38So let me get this straight - we’re scared of a pill that’s been studied in millions of pregnancies, but fine with letting moms spiral into suicide because ‘natural is better’? 🤡
Also, paroxetine is the outlier, not the rule. Stop using it like it’s the default. Sertraline’s the MVP here.
Pawittar Singh
November 30, 2025 AT 01:52I was on Zoloft during both my pregnancies and my kids are now 7 and 9 - thriving, smart, happy, no autism, no delays, just normal little humans who love dinosaurs and pancakes.
People act like meds are poison, but untreated depression? That’s the real poison. You’re not failing your baby by taking care of yourself - you’re saving them. 💪❤️
Josh Evans
December 1, 2025 AT 10:44Honestly? I stopped my meds when I got pregnant. Thought I was being ‘strong.’
Three weeks in, I couldn’t get out of bed. Didn’t shower for five days. My partner had to feed me cereal with a spoon.
Started back on sertraline. Life came back. My baby’s healthy. I’m alive. Don’t be me.
Allison Reed
December 1, 2025 AT 22:02The data is clear. Untreated depression is a public health crisis in pregnancy. SSRIs are not the problem - stigma is.
Doctors need to stop whispering about ‘risks’ and start shouting about ‘benefits.’
And if you’re worried about your baby? Talk to a perinatal psychiatrist. Not Reddit. Not your aunt. A professional.
Jacob Keil
December 3, 2025 AT 02:18You ever think maybe the real issue is capitalism? We’re so disconnected from community that women are told to pop pills instead of getting real support? Therapy costs 200 bucks an hour. Daycare costs more than rent. Of course people take meds. They’re not choosing poison - they’re choosing survival in a broken system.
Rosy Wilkens
December 3, 2025 AT 23:27Did you know the FDA panel was influenced by Big Pharma? The same companies that make SSRIs also fund half the ‘safe’ studies. The CDC is in bed with them. They’re hiding the truth. Your baby’s brain is being rewired. Look at the autism rates - they’ve tripled since 2000. Coincidence? I think not.
Andrea Jones
December 4, 2025 AT 16:27Okay but can we talk about how wild it is that people think it’s ‘natural’ to be emotionally shattered for nine months? Like, you wouldn’t let someone with diabetes go without insulin. Why is mental health different?
Also - breastfeeding on sertraline? Total non-issue. My milk tasted like normal milk. Baby slept like a champ.
Justina Maynard
December 5, 2025 AT 17:05I’m not anti-medication. I’m anti-ignoring the emotional labor.
Why is it easier to hand someone a pill than to build a village? Why are we so obsessed with fixing symptoms instead of fixing the conditions that make people sick?
I took sertraline during pregnancy. I also had a doula, a therapist, a partner who cooked, and a friend who brought soup every Tuesday.
The pill helped. The village saved me.
Evelyn Salazar Garcia
December 6, 2025 AT 21:10Stop pushing pills. Just stop.
Clay Johnson
December 8, 2025 AT 02:08The fear isn't about the drug. It's about the loss of control. We are told to surrender our bodies to medicine. To trust institutions that have lied before. To silence our instincts. But what if the instinct is right? What if the system is wrong?
Jermaine Jordan
December 8, 2025 AT 08:16THIS IS A LIFE OR DEATH ISSUE.
Women are dying. Not from SSRIs. From silence. From shame. From being told to ‘just be positive’ while their soul is on fire.
Every time someone says ‘just meditate’ instead of prescribing sertraline, they’re gambling with a life. Don’t be that person.
Chetan Chauhan
December 8, 2025 AT 16:18Umm actually sertraline is just a rebranded version of an old Soviet antidepressant. And guess what? They stopped using it in Russia because it made people emotionally numb. So maybe ‘safest’ doesn’t mean ‘best’? Just sayin’.
Phil Thornton
December 10, 2025 AT 01:52I took Lexapro during pregnancy. My son is 4. He plays soccer. He loves cheese. He calls me ‘mommy’.
That’s all you need to know.