Teriparatide vs Abaloparatide: What You Need to Know About Anabolic Agents for Osteoporosis

When bone loss goes beyond prevention
Most people with osteoporosis start with pills that slow bone breakdown-bisphosphonates, denosumab, or similar drugs. But if your bones are already severely weakened, those won’t rebuild what’s been lost. That’s where anabolic agents like teriparatide and abaloparatide come in. These aren’t just more potent versions of older drugs. They’re fundamentally different: they actually trigger your body to make new bone. Think of it like this: antiresorptive drugs are the brakes. Anabolic agents are the gas pedal. If you’ve had multiple fractures, your T-score is below -3.0, or your doctor says you’re at very high risk, this is the next step. Both teriparatide and abaloparatide are daily injections. Both are used for no more than 18 to 24 months. Both are followed by a long-term antiresorptive drug to lock in the gains. But the differences between them? They matter-especially if you’re trying to avoid another fracture or manage side effects.How teriparatide and abaloparatide work
Teriparatide is a piece of human parathyroid hormone (PTH 1-34). It’s been around since 2002, the first drug of its kind approved by the FDA. Abaloparatide, approved in 2017, is a synthetic copy of a different hormone-PTHrP-that mimics how your body naturally builds bone. The key difference? They bind to the same receptor on bone cells, but in slightly different ways. Abaloparatide prefers the RG conformation of the receptor, which leans more toward bone formation and less toward bone breakdown. Teriparatide activates both sides of the receptor more evenly. That’s why abaloparatide causes less hypercalcemia (high calcium in the blood) and appears to build more bone in the hip. In the ACTIVE trial, abaloparatide reduced new vertebral fractures by 86% compared to placebo. Teriparatide reduced them by about 65%. The hip fracture numbers were even more telling: abaloparatide cut hip fractures by 43% more than teriparatide in a 2024 real-world study of over 43,000 women.Which one builds more bone?
Bone mineral density (BMD) gains tell part of the story. At 18 months:- Lumbar spine: Both increase BMD by about 9-10%. Abaloparatide leads slightly at 6 months, but by 18 months, the difference fades.
- Femoral neck: Abaloparatide wins. +2.93% vs +1.49% with teriparatide.
- Total hip: Abaloparatide again leads. +3.41% vs +2.04%.
Safety: Side effects you can’t ignore
Both drugs can cause dizziness, nausea, and leg cramps. About 1 in 3 people report injection site reactions. But the big difference is hypercalcemia. Teriparatide causes high blood calcium in 6.4% of users. Abaloparatide? Only 3.4%. That’s nearly half the rate. For people with kidney issues, a history of kidney stones, or who are older and more sensitive to calcium shifts, this isn’t a minor detail-it’s a dealbreaker. Real-world patient reports back this up. On osteoporosis forums, users switching from teriparatide to abaloparatide often say their calcium levels normalized within weeks. One Reddit user wrote: “I was getting dizzy and nauseous every day. My doctor said it was the calcium. Switched to abaloparatide-no more issues.” Dizziness is also more common with teriparatide: 41% vs 29% with abaloparatide. That’s a problem if you’re already at risk for falls.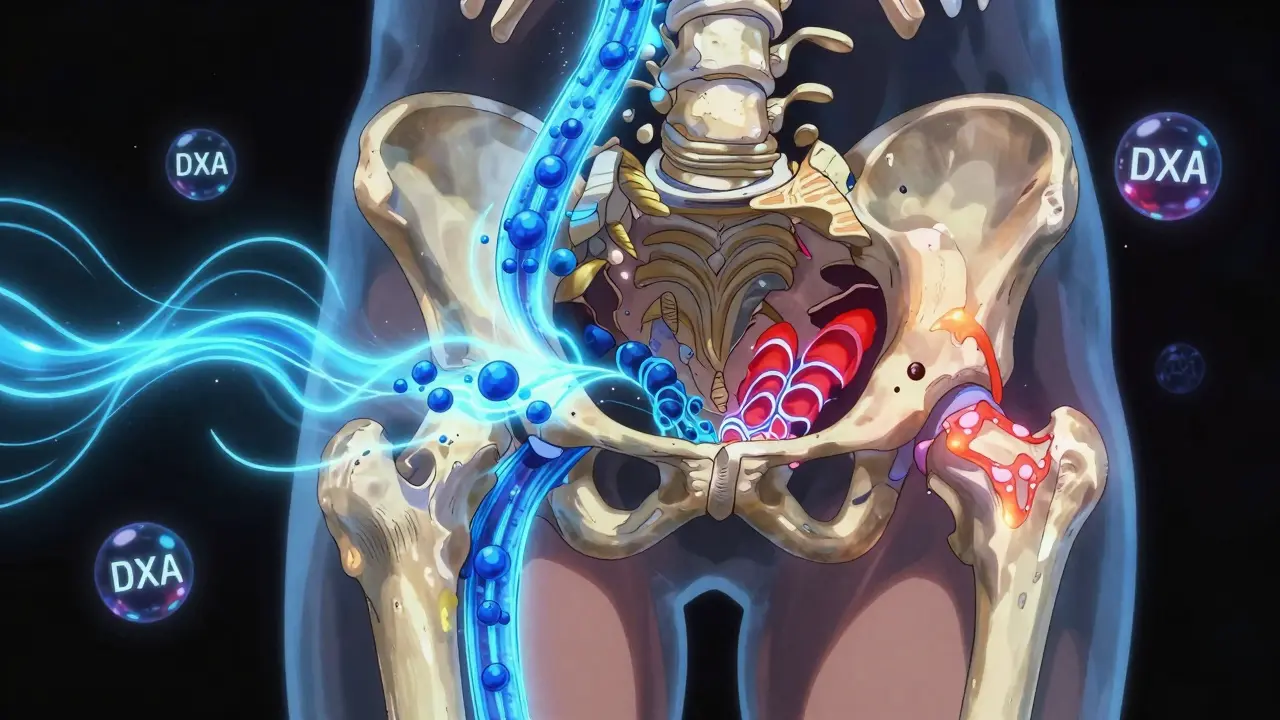
Cost and access
Here’s where things get messy. As of early 2025, teriparatide (now generic) costs about $4,200 per month. Abaloparatide? Still brand-name, around $5,750. That’s a 37% difference. Insurance coverage is a huge barrier. In 2023, 44% of abaloparatide users reported prior authorization denials or high copays. Only 28% of teriparatide users had the same issue. The introduction of generic teriparatide in January 2024 changed the game. By 2025, its price is expected to drop another 40%. That makes teriparatide the clear choice for cost-sensitive patients-especially if their hip T-score isn’t critically low.Who gets which drug?
There’s no one-size-fits-all answer. But guidelines from the American Association of Clinical Endocrinologists (AACE) in 2023 give clear direction:- Start with teriparatide if you’re cost-conscious, have no prior hip fractures, and your main concern is spine or general bone density.
- Choose abaloparatide if you have a hip T-score ≤ -3.0, a history of nonvertebral fractures, or you’ve had hypercalcemia on other treatments.
How the treatment works in practice
Both drugs are injected daily under the skin, usually in the thigh or abdomen. They come in pre-filled pens. You need to keep them refrigerated. Most people get used to the routine within a few weeks. The first month is the hardest. About 78% of patients need help with injection technique, timing, or managing dizziness after the shot. Orthostatic hypotension-feeling lightheaded when standing up-is common, especially in the first hour after injection. Most doctors recommend sitting or lying down for 30 minutes after each dose. You won’t see results right away. DXA scans at 6 months show if you’re responding. If your lumbar spine BMD hasn’t increased by at least 3%, your doctor may question whether the drug is working for you.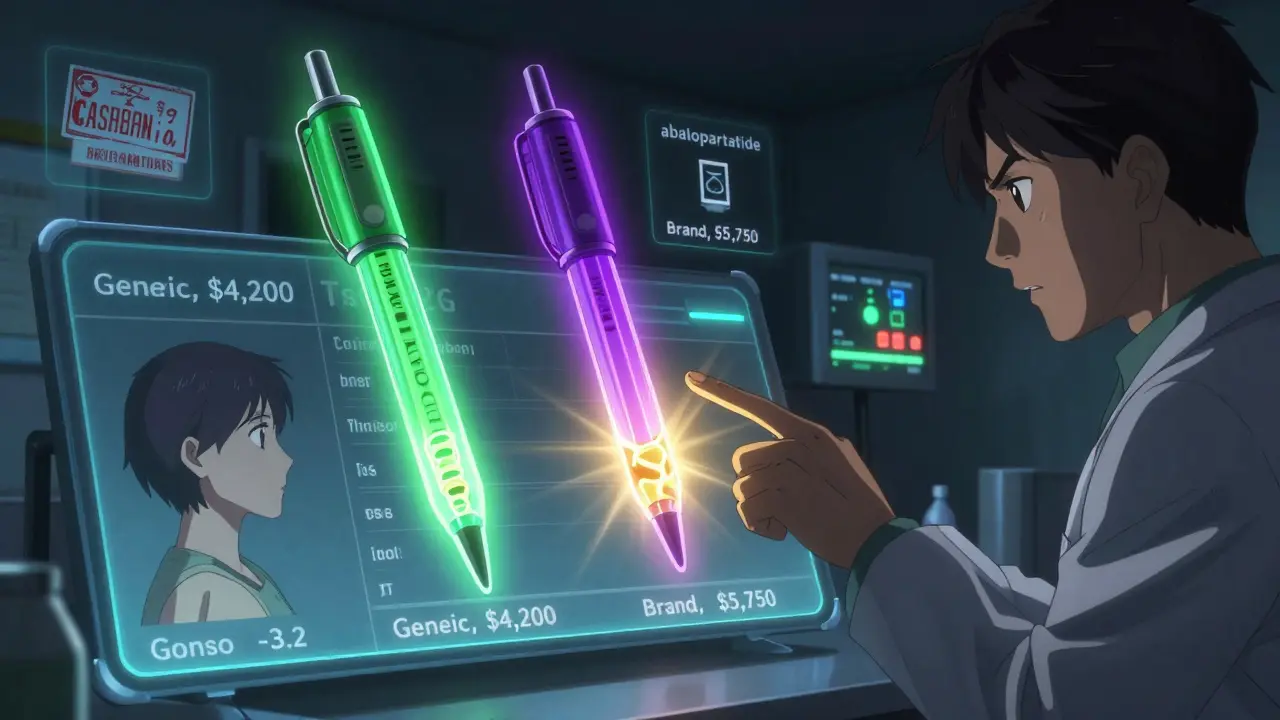
What happens after 18 months?
Neither drug can be used longer than 24 months. That’s because long-term use may increase the risk of osteosarcoma (a rare bone cancer) in animal studies. We don’t see that in humans, but the FDA still limits use. That’s why the next step matters more than the first. The ACTIVE-EXTEND trial showed that after 18 months of abaloparatide, switching to alendronate (a bisphosphonate) kept the gains. At 3.5 years, 68% of patients kept their total hip T-score above -2.5. Only 52% did if they’d been on placebo then alendronate. The same applies to teriparatide. You don’t stop treatment-you transition. That’s now standard practice. The goal isn’t just to build bone-it’s to keep it.What’s coming next?
The future of these drugs isn’t just about picking between two daily injections. Radius Health is testing a weekly version of abaloparatide. Phase 3 trials ended in December 2023. Results are expected in late 2025. If approved, that could dramatically improve adherence. The FDA has also signaled it’s open to extending treatment beyond 24 months-something that could change the game for patients with chronic, progressive osteoporosis. Meanwhile, the market is shifting. Teriparatide still leads in sales, but abaloparatide is growing fast. By 2028, anabolic agents are expected to make up 41% of the osteoporosis market, up from 32% today. Why? Because we’re aging. By 2030, 1 in 5 Americans will be over 65. And 10.2 million already have osteoporosis severe enough to need these drugs.Final thoughts: It’s not about the drug-it’s about the person
Choosing between teriparatide and abaloparatide isn’t about which one is “better.” It’s about which one is better for you. If you’re older, have a history of fractures, high risk of falling, or trouble with calcium levels-abaloparatide’s safety edge and hip benefits make it the stronger choice. If you’re younger, have good insurance, or are trying to minimize out-of-pocket costs-teriparatide still delivers strong results with a proven track record. Either way, this isn’t a lifelong pill. It’s a targeted, time-limited push to rebuild bone before switching to maintenance therapy. And for people who’ve already lost too much, it’s one of the most powerful tools we have.Frequently Asked Questions
Can I take teriparatide or abaloparatide if I’ve had radiation therapy to the spine?
No. Both drugs are contraindicated in people with a history of radiation therapy to the skeleton, including the spine or pelvis. This is because animal studies showed an increased risk of bone cancer after exposure to both radiation and these drugs. If you’ve had radiation, your doctor will choose an alternative treatment like denosumab or a bisphosphonate.
Do I need to take calcium and vitamin D with these drugs?
Yes. Both teriparatide and abaloparatide require adequate calcium and vitamin D to work. Your doctor will check your levels before starting. If your vitamin D is below 30 ng/mL or your calcium is low, you’ll need supplements. Without them, the drugs won’t build bone effectively-and your risk of hypercalcemia increases.
Why can’t I use these drugs longer than 2 years?
Animal studies showed a rare type of bone cancer (osteosarcoma) in rats given high doses for long periods. While no cases have been confirmed in humans, the FDA limits treatment to 24 months as a precaution. After that, you switch to an antiresorptive drug like alendronate or denosumab to maintain bone density.
Can men use teriparatide or abaloparatide for osteoporosis?
Yes. Both drugs are approved for men with severe osteoporosis who are at high risk of fracture. Studies show similar improvements in bone density and fracture reduction in men as in women. However, most clinical trial data comes from postmenopausal women, so real-world experience in men is more limited.
What if I miss a dose?
If you miss a dose, take it as soon as you remember-but only if it’s the same day. Don’t double up the next day. Missing one dose won’t ruin your results, but consistency matters. Try setting a daily phone alarm or linking the injection to a routine like brushing your teeth. Missing multiple doses reduces effectiveness and increases fracture risk.
Is there a generic version of abaloparatide?
No. Abaloparatide (Tymlos) is still under patent protection and only available as a brand-name drug. Generic teriparatide became available in January 2024, which is why its price has dropped significantly. There are no generic alternatives to abaloparatide expected before 2028.


Comments
Selina Warren
January 18, 2026 AT 23:45I switched from teriparatide to abaloparatide after my third vertebral fracture and holy hell, what a difference. No more dizziness, no more calcium spikes, and my hip BMD actually went up instead of plateauing. This isn’t just science-it’s survival. 💪
Robert Davis
January 20, 2026 AT 17:46The data looks good on paper, but let’s be real-pharma is just selling us another expensive injection. The real problem is we’re treating osteoporosis like it’s a glitch to be fixed instead of a symptom of a broken system. We need better nutrition, more sunlight, less processed food.
Eric Gebeke
January 21, 2026 AT 09:52You people don’t even know what you’re talking about. Teriparatide has been used for 20+ years with zero confirmed osteosarcoma cases in humans. Abaloparatide’s ‘superiority’ is based on industry-funded trials. The FDA limit? That’s not safety-it’s liability. Don’t fall for the hype.
Chuck Dickson
January 22, 2026 AT 00:32Hey everyone-just wanted to say if you’re on one of these meds, you’re not alone. I’ve been on abaloparatide for 14 months now. The first month sucked-I was dizzy every time I stood up. But I started doing my injections right after my morning coffee, sitting down for 45 mins, and it got way better. You got this. And yes, vitamin D is non-negotiable. I take 5000 IU daily now. 🙌
rachel bellet
January 22, 2026 AT 11:36The ACTIVE trial’s fracture reduction metrics are statistically significant but clinically marginal when contextualized within the broader osteopenic population. The number needed to treat (NNT) for nonvertebral fracture avoidance with abaloparatide exceeds 15, whereas the incremental cost-effectiveness ratio (ICER) surpasses $250,000 per QALY. This is not cost-effective population-level care.
Pat Dean
January 23, 2026 AT 00:50I don’t trust these drugs. They’re all just Big Pharma’s way of keeping old people hooked on pills. My uncle took teriparatide and ended up in the ER with kidney stones. Now they want us to pay $5K a month for a ‘better’ version? No thanks. I’m going to drink bone broth and do yoga.
Joni O
January 24, 2026 AT 17:33i just started abaloparatide last week and honestly? i’m scared. the injection hurts, i keep forgetting, and i’m worried about the dizziness. but my dr said if i don’t do something, i might break my hip. anyone else feel like this? pls tell me it gets easier...
Max Sinclair
January 25, 2026 AT 16:51Joni, it gets better. Seriously. I was in the same spot. Set a reminder on your phone labeled ‘Bone Boost Time’ and keep a little chair next to your bed for after the shot. First two weeks are rough, but your body adapts. And you’re doing the right thing. Proud of you for starting.
christian Espinola
January 26, 2026 AT 02:03Funny how they never mention the FDA’s own warning about osteosarcoma in rats. You think they’d tell you if your injection could give you bone cancer? Nah. They’ll sell you the pen, then blame you for not reading the 50-page insert. Wake up.
Dayanara Villafuerte
January 27, 2026 AT 01:04LMAO at the people saying ‘just drink bone broth.’ 🤦♀️ I’ve been on both. Abaloparatide saved my hip. I’m not dying because I didn’t eat enough collagen. Also, generic teriparatide? $4.2K/month? That’s a joke. My insurance paid $120. Y’all need to check your coverage before you rant. 🙄
kenneth pillet
January 28, 2026 AT 02:40I’m on teriparatide. Cost is half. Side effects are manageable. My spine BMD went up 11%. Hip stayed stable. Switching to abaloparatide for a 1.5% hip gain at triple the cost? Not worth it for me. Insurance approved both. I chose the one that didn’t make me broke.