Asthma vs. COPD: Key Differences in Symptoms and Treatment

Many people think asthma and COPD are the same thing - both make you wheeze and struggle to breathe. But they’re not. One is often manageable with the right care. The other slowly wears your lungs down, year after year. If you’re over 40 and have been told you have asthma but aren’t improving, you might actually have COPD. Or worse - you could have both. Knowing the difference isn’t just helpful. It can save your life.
How Your Breathing Feels: Asthma vs. COPD
If you have asthma, your breathing problems come and go. You might wake up gasping at 3 a.m. after a night of coughing, then feel fine by noon. You can run, laugh, or climb stairs without trouble - until you’re near pollen, cold air, or smoke. Then, suddenly, your chest tightens. Your lungs feel like they’re squeezing shut. That’s asthma. It’s triggered. It’s reversible. And it often starts in childhood.
COPD is different. You don’t wake up feeling fine. You wake up already tired. Your cough is constant - not just in the morning, but all day. You’re coughing up phlegm, thick and yellow or gray. You get winded walking to the mailbox. Climbing stairs feels like hiking a mountain. There’s no break. No good day. Even when you’re not sick, your lungs are working harder than they should. And it only gets worse.
One clear sign of COPD? Bluish lips or fingernails. That’s cyanosis - your body isn’t getting enough oxygen. It doesn’t happen in asthma. If you’ve never seen it, picture someone struggling to breathe after years of smoking. Their skin looks tired. Their lips look purple. That’s COPD. Asthma doesn’t do that.
Who Gets It - And When
Asthma usually shows up early. Half of all cases are diagnosed before age 10. Eighty percent are caught by age 30. It’s common in kids with allergies, eczema, or a family history. If your mom had asthma, you’re more likely to get it.
COPD? Almost never shows up before 40. Nine out of ten people diagnosed are over 45. It’s the result of long-term damage - mostly from smoking. About 90% of COPD cases are tied to cigarettes. Even if you quit 20 years ago, the damage is still there. And it keeps getting worse.
There’s a twist: some people with asthma smoke. And some people with COPD have allergies. That’s where things get messy. This mix is called Asthma-COPD Overlap Syndrome, or ACOS. It affects 15 to 25% of people with obstructive lung disease. These patients have worse symptoms than those with just asthma or just COPD. They end up in the ER more often. Their lungs decline faster.

How Doctors Tell Them Apart
Doctors don’t guess. They test. The most common tool? Spirometry. You blow into a tube as hard and fast as you can. The machine measures how much air you can push out in one second (FEV1). Then you get a puff of bronchodilator - a quick-acting inhaler. You wait 15 minutes. You blow again.
If your FEV1 improves by 12% or more? That’s asthma. About 95% of asthma patients show this kind of reversibility. If your numbers barely change? That’s COPD. Only 15% of COPD patients show meaningful improvement.
Another test? Fractional exhaled nitric oxide, or FeNO. You breathe into a device that measures inflammation in your airways. If your FeNO is above 50 ppb? High chance of asthma. It’s caused by eosinophils - a type of white blood cell that flares up with allergies. COPD patients usually have FeNO below 25 ppb. Blood tests for eosinophils help too. Counts above 300 cells/μL point to asthma or ACOS. Below 100? Likely pure COPD.
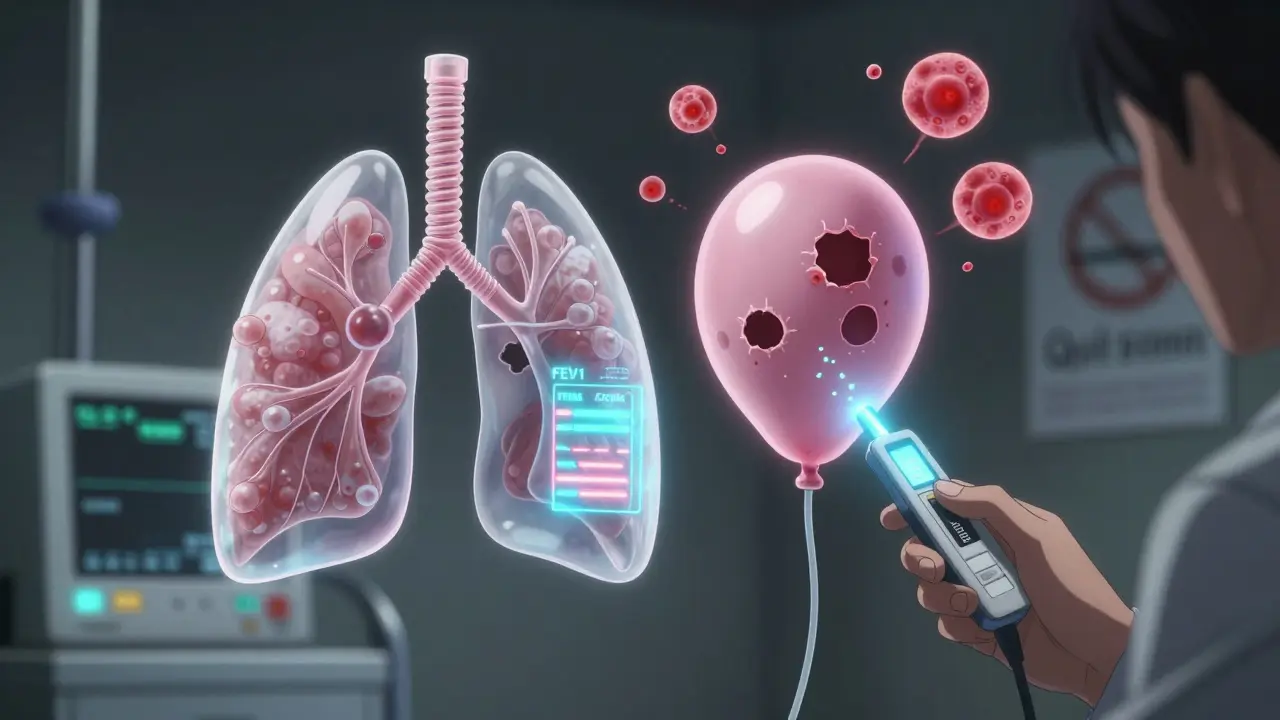
CT scans show even more. In COPD, 75% of patients have emphysema - holes in the lungs where air sacs have collapsed. In asthma? Only 5% show this. It’s like comparing a deflated balloon (COPD) to a kinked hose (asthma).
Treatment: What Works - And What Doesn’t
Asthma treatment is all about control. Start with a rescue inhaler - usually albuterol - for sudden attacks. If you need it more than twice a week? You need a daily controller. That’s usually an inhaled corticosteroid. It reduces swelling in your airways. For severe cases, biologics like omalizumab or mepolizumab target specific immune cells. These shots cut flare-ups by half in people with allergic asthma.
COPD? Rescue inhalers help, but they’re not enough. First-line treatment is long-acting bronchodilators - either LABAs or LAMAs. These open your airways for 12 to 24 hours. Steroids? Only if you’re having frequent flare-ups. Too many steroids in COPD can cause pneumonia and bone loss. That’s why doctors avoid them unless necessary.
Pulmonary rehab? Huge for COPD. Patients who do it walk 54 meters farther in six minutes. That’s life-changing. For asthma? Only 12 meters. Why? Because their lungs are already healthy between attacks. Rehab doesn’t fix what’s not broken.
And smoking? Quitting is the single most important thing for COPD. The Lung Health Study showed quitting cuts disease progression by 50%. For asthma? Smoking doesn’t change much - unless you already have COPD. Then it’s a double hit.
Prognosis: What to Expect Long-Term
Asthma has a strong track record. If you’re diagnosed young and stick to your treatment, your 10-year survival rate is 92%. Most people live full, active lives. Deaths from asthma have dropped to about 3,500 per year in the U.S. - thanks to better meds and awareness.
COPD? Less hopeful. The 10-year survival rate for moderate COPD is 78%. It kills 152,000 Americans every year - the fourth leading cause of death. Hospitalizations happen 7 times more often than in asthma. One study found COPD patients have nearly one exacerbation per year. Asthma? Just one every eight months.
There’s one scary twist: long-term asthma can turn into fixed airflow obstruction. About 15-20% of people with asthma for more than 20 years develop permanent lung damage - just like COPD. That’s why it’s dangerous to ignore asthma, even if it seems mild.
When to Worry - And What to Do Next
If you’re under 40 and have wheezing, coughing at night, or symptoms after exercise - get tested for asthma. Allergies? Family history? Even more reason.
If you’re over 45, smoked for years, and have a daily cough with phlegm - don’t brush it off as "just a smoker’s cough." Get a spirometry test. If you’ve been told you have asthma but your inhaler doesn’t help much? You might have COPD - or ACOS.
ACOS is tricky. You might need triple therapy: a LABA, a LAMA, and an inhaled steroid. But evidence is still limited. Your doctor should monitor you closely. You’re at higher risk for flare-ups, hospital stays, and faster decline.
Don’t wait for a crisis. If you’re struggling to breathe, even a little, see a pulmonologist. Don’t rely on your GP alone. They miss the diagnosis in 30% of cases over age 40.
And if you smoke? Quit. Today. No excuses. It’s the only thing that slows COPD. It helps asthma too - especially if you’re already on steroids.
Can you have asthma and COPD at the same time?
Yes. This is called Asthma-COPD Overlap Syndrome (ACOS). It affects 15-25% of people with obstructive lung disease. These patients often have a history of asthma and smoking. Their symptoms are worse than either condition alone - more frequent flare-ups, faster lung decline, and higher hospitalization rates. Treatment usually combines asthma and COPD therapies, including long-acting bronchodilators and inhaled steroids.
Is COPD curable?
No. COPD is not curable. The lung damage - especially from emphysema - is permanent. But it is manageable. Quitting smoking, using bronchodilators, doing pulmonary rehab, and avoiding triggers can slow progression and improve quality of life. The goal isn’t to cure it, but to keep you breathing as well as possible for as long as possible.
Can asthma turn into COPD?
Asthma doesn’t automatically turn into COPD. But long-standing, poorly controlled asthma can cause permanent airway changes - called fixed airflow obstruction. About 15-20% of people with asthma for more than 20 years develop this. Smoking speeds this up dramatically. So if you have asthma and smoke, your risk of permanent lung damage rises sharply.
What’s the best test to tell asthma from COPD?
The gold standard is spirometry with a bronchodilator challenge. If your FEV1 improves by 12% or more after using an inhaler, it’s likely asthma. If it doesn’t change much, it’s probably COPD. FeNO testing (measuring nitric oxide in your breath) and blood eosinophil counts add more clarity. High FeNO (>50 ppb) and high eosinophils (>300 cells/μL) point to asthma. Low levels suggest COPD.
Why do some people with asthma need steroids but COPD patients don’t?
Asthma is driven by eosinophilic inflammation - a type of immune response that responds well to steroids. COPD is mostly caused by neutrophilic inflammation from smoke and pollution. Steroids don’t work as well here. In fact, long-term steroid use in COPD increases risk of pneumonia, bone loss, and diabetes. So doctors only add them to COPD treatment if you have frequent flare-ups - and even then, they use the lowest effective dose.
If you’ve been told you have asthma but your inhaler isn’t working like it should - don’t assume you’re not using it right. Ask for a full lung function test. If you’re over 45 and have a chronic cough, get checked for COPD - even if you quit smoking years ago. Your lungs remember. And so should you.



Comments
Skye Kooyman
January 26, 2026 AT 18:30I had no idea asthma and COPD could look so different until my dad got diagnosed. He’s 58, smoked for 30 years, and they kept calling it asthma for years. That blue tint around his lips? I thought he was just cold.
Turns out, it was COPD. Spirometry was the only thing that nailed it. His inhaler did nothing. Now he’s on LAMA and doing rehab. Life’s still hard, but he’s breathing better.
Don’t ignore the cough. It’s not "just a smoker’s thing."
Shawn Raja
January 28, 2026 AT 00:03So let me get this straight - we’ve got a disease that’s basically your lungs screaming "I quit!" after 30 years of you treating them like a cigarette ashtray... and we’re still surprised people die from it?
Meanwhile, asthma is like your body throwing a tantrum when it sees a cat. One puff of albuterol and it’s back to yoga.
Stop treating chronic lung damage like it’s seasonal allergies. Quitting smoking isn’t a suggestion - it’s the only thing that doesn’t involve a funeral.
Also, why do we still call it "COPD"? Sounds like a bad sci-fi movie. "The Rise of the Chronic Obstructive People."
Ryan W
January 29, 2026 AT 17:24According to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2024 guidelines, the FEV1/FVC ratio <0.7 post-bronchodilator remains the diagnostic criterion for COPD, irrespective of symptoms.
Meanwhile, the 2023 GINA report emphasizes that asthma is defined by variable expiratory airflow limitation with airway hyperresponsiveness and eosinophilic inflammation.
FeNO >50 ppb has 89% specificity for eosinophilic asthma - yet primary care providers still prescribe ICS empirically in COPD patients without biomarker confirmation.
This is why mortality rates remain high. Misdiagnosis isn’t negligence - it’s systemic incompetence.
Stop relying on GP intuition. Demand spirometry. Demand FeNO. Demand eosinophil counts.
If you’re over 40 and smoke? You’re not "just wheezing." You’re in a slow-motion respiratory collapse.
And if you think biologics are for asthma only? You’re wrong. ACOS patients are the fastest-growing subgroup needing dupilumab.
Stop guessing. Start testing.
Allie Lehto
January 31, 2026 AT 11:25OMG I JUST REALIZED MY DAD HAS COPD AND WE THOUGHT IT WAS JUST ASTHMA 😭
He’s been coughing for 15 years and we kept buying him more albuterol like it was candy 🤦♀️
Now I’m crying because I didn’t know smoking for 40 years = permanent lung damage 😭
Why didn’t anyone TELL US?!
Also I think I have asthma? I wheeze when I run 😭
But I’m vegan and yoga every day so it’s probably just stress? 😅
PLS HELP I’M SCARED
Napoleon Huere
February 2, 2026 AT 11:19Here’s the real question nobody asks: Why do we treat asthma like a medical condition and COPD like a moral failure?
Asthma gets sympathy. COPD gets judgment.
But what if the person with COPD started smoking because their job was 12-hour shifts at a factory with no health insurance? What if they were 16 and thought it was cool?
What if they were depressed and the only thing that calmed them was a cigarette?
We don’t blame the kid with asthma for having allergies. We don’t say "they should’ve just avoided cats."
So why do we say "they should’ve just quit" to someone with COPD?
It’s not about blame. It’s about care.
And care means giving people tools - not shame.
Rehab works. Bronchodilators help. Quitting matters.
But the system has to meet people where they are - not where we wish they’d been.
Shweta Deshpande
February 4, 2026 AT 03:50Wow this is so important! I’m from India and here so many people think coughing all day is just "normal" because they’ve smoked for decades. My uncle had COPD and we didn’t know until he collapsed. He was 52.
They gave him oxygen at the hospital and said "this is what happens when you smoke." No tests, no spirometry, no rehab.
I’m so glad this post exists. Please, if you’re reading this and you’re over 40 and smoke - go get tested. Even if you quit 10 years ago. Your lungs remember.
And if you have asthma and smoke - please, for the love of your future self, stop. It’s not just about COPD. It’s about being able to play with your grandkids without gasping.
I’m sending so much love to everyone fighting this. You’re not alone. 💛
Aishah Bango
February 5, 2026 AT 21:41People who smoke and then act shocked they have lung disease are the reason healthcare costs are insane.
You knew the risks. You chose it. Now you want a biologic? A rehab program? A miracle?
No. You get what you earned.
Stop pretending it’s not your fault.
And if you have asthma and smoke? You’re not just risking your lungs - you’re wasting medicine that could help someone who didn’t choose this.
Take responsibility. Or shut up.
Simran Kaur
February 6, 2026 AT 02:34I just lost my aunt to COPD last month. She was 64. She smoked for 40 years but also had asthma since she was 8. They called it "asthma" for 25 years until she couldn’t walk to the bathroom without stopping.
She never got a proper spirometry. The doctor said "she’s just wheezing."
She cried every night because she couldn’t hold her grandbaby without gasping.
My heart is broken.
If you’re reading this and you have a cough that won’t go away - please, go to a pulmonologist. Not your GP. Not a clinic. A specialist.
They can help. Even if it’s too late for you - it might be early enough for someone you love.
Don’t wait until it’s too late.
I’m crying as I type this.
And I’m sending you all so much strength.
You’re not alone. 💕
Neil Thorogood
February 6, 2026 AT 21:45Bro. I’ve been on 3 inhalers since I was 12. Asthma. Allergic. Fine.
Then I turned 42. Started coughing 24/7. Couldn’t climb stairs. Blue lips? Yeah. That’s not a filter. That’s real.
Got tested. COPD. ACOS. The combo.
They told me to quit smoking. I did. 18 months ago.
Rehab. LAMA. LABA. Steroid now because I flare up every winter.
Still can’t run. Still wheeze. But I can carry my groceries now.
And I can hold my daughter without gasping.
So yeah. It’s not a cure.
But it’s not the end either.
Quit. Get tested. Do rehab.
You’re not broken.
You’re just behind.
And it’s never too late to catch up. 💪🫁