Fracture Prevention: How Calcium, Vitamin D, and Bone-Building Medications Actually Work

Every year, over 2 million fractures happen in the U.S. because of weak bones. Most of these aren’t from car crashes or sports injuries. They’re from simple falls - stepping off a curb, slipping on a wet floor, even just rolling over in bed. And for people over 65, especially women after menopause, one of these falls can change everything. A hip fracture often means losing independence. A spine fracture can make you shrink, hurt constantly, and struggle to breathe. The good news? You don’t have to wait for that first break to act. The right mix of calcium, vitamin D, and bone-building medications can cut your risk dramatically - but only if you use them the right way.
Calcium and Vitamin D Together Work - Alone, They Don’t
You’ve probably heard that calcium builds strong bones. And vitamin D helps your body absorb it. That’s true. But here’s the catch: taking vitamin D by itself? It won’t stop fractures. A major 2019 review of over 34,000 people found no benefit at all. Even taking 800 IU of vitamin D daily didn’t lower the chance of breaking a hip or any other bone. The same goes for low-dose calcium - 1,000 mg or less - without vitamin D. The Women’s Health Initiative, which tracked nearly 36,000 postmenopausal women, showed no reduction in fractures with 400 IU of vitamin D and 1,000 mg of calcium. That’s the dose most over-the-counter supplements offer. It’s not enough.
But when you combine 800-1,000 IU of vitamin D3 with 1,000-1,200 mg of calcium daily, the picture changes. Six large studies with nearly 50,000 people showed a 6% lower risk of any fracture and a 16% lower risk of hip fracture over six years. This isn’t magic. It’s biology. Your bones are constantly being broken down and rebuilt. Calcium is the raw material. Vitamin D is the delivery system. Without enough of both, your body can’t repair bone fast enough to keep up with natural loss - especially after age 50.
But not everyone needs this combo. The real benefit shows up in people who are deficient. If your blood vitamin D level is below 20 ng/mL, or you’re eating less than 700 mg of calcium a day, adding both supplements makes a huge difference. The landmark 1992 Chapuy trial found a 43% drop in hip fractures among nursing home residents with severe deficiency. But in healthy, active older adults with normal levels? The RECORD trial showed no benefit. That’s why testing your vitamin D level before starting supplements isn’t optional - it’s essential.
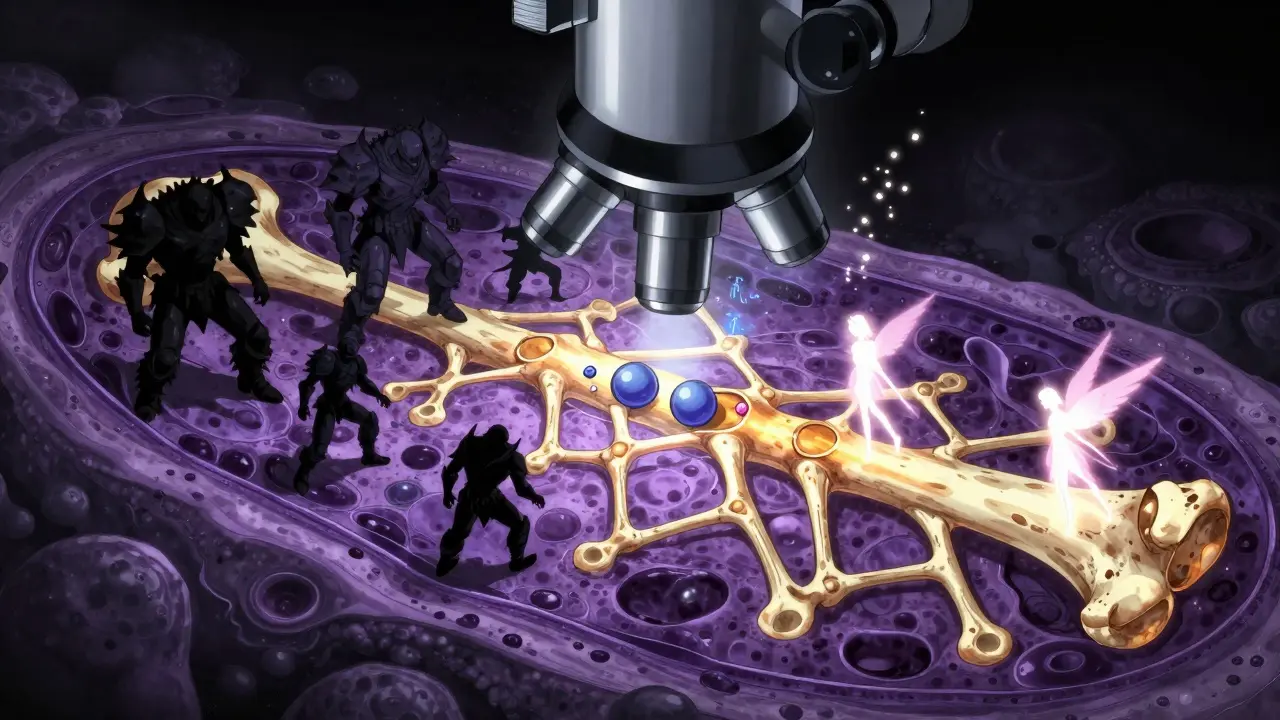
Bone-Building Medications Are the Real Game-Changers
If you’ve already had a fracture, or your bone density scan shows osteoporosis, supplements alone won’t cut it. That’s where medications come in. These aren’t just “bone boosters.” They’re targeted tools that either slow bone loss or rebuild it.
Bisphosphonates - like alendronate (Fosamax) and zoledronic acid (Reclast) - are the most common. They work by putting the brakes on cells that break down bone. In the Fracture Intervention Trial, alendronate cut vertebral fractures by 44%. Zoledronic acid, given as a yearly IV infusion, reduced hip fractures by 41% over 18 months. These drugs work. But they’re not perfect. About 22% of people stop taking oral bisphosphonates within a year because of stomach upset, heartburn, or jaw pain. That’s why many doctors now start with the IV version - no daily pill, no gut irritation.
Then there’s denosumab (Prolia), a monthly injection that blocks a protein that triggers bone breakdown. It reduces spine fractures by 68% and hip fractures by 40%. But if you miss a dose, bone loss can rebound fast. You can’t just stop it cold - you need to switch to another medication.
The newest class - anabolic agents - actually builds new bone. Teriparatide (Forteo) and romosozumab (Evenity) stimulate bone-forming cells. Teriparatide cuts vertebral fractures by 65%. Romosozumab, approved in 2019, reduces spine fractures by 73% in the first year. But these are expensive and usually limited to one or two years of use. After that, you move to a bisphosphonate or denosumab to hold onto the gains.
Here’s the reality: supplements help prevent bone loss. Medications fix it. If your FRAX® score shows a 20% or higher chance of a major fracture in 10 years, you’re a candidate for medication - not just pills from the drugstore.
The Hidden Risks: When Help Becomes Harm
Nothing in medicine is risk-free. Calcium supplements, even when they work, come with trade-offs. The Women’s Health Initiative found a 17% higher risk of kidney stones. Another analysis linked daily calcium doses over 1,000 mg to a slight increase in heart attack risk. That’s why getting calcium from food - dairy, leafy greens, canned salmon with bones - is always better than pills. If you must supplement, take no more than 600 mg at a time. Your body can’t absorb more.
Bisphosphonates carry rare but serious risks. Osteonecrosis of the jaw - where bone in the jaw dies - happens in fewer than 1 in 10,000 people per year. Atypical femur fractures - a snap in the thigh bone without trauma - occur in about 1 in 1,000 after five years of use. These aren’t common, but they’re real. That’s why dentists now ask about bisphosphonate use before pulling teeth. And why doctors recommend a “drug holiday” after 3-5 years for low-risk patients.
Vitamin D overdose is rare, but it happens. Taking more than 4,000 IU daily long-term can raise blood calcium levels, leading to nausea, confusion, or even kidney damage. The Endocrine Society recommends testing levels before starting, then checking again in 3-6 months. Don’t guess. Don’t mega-dose.
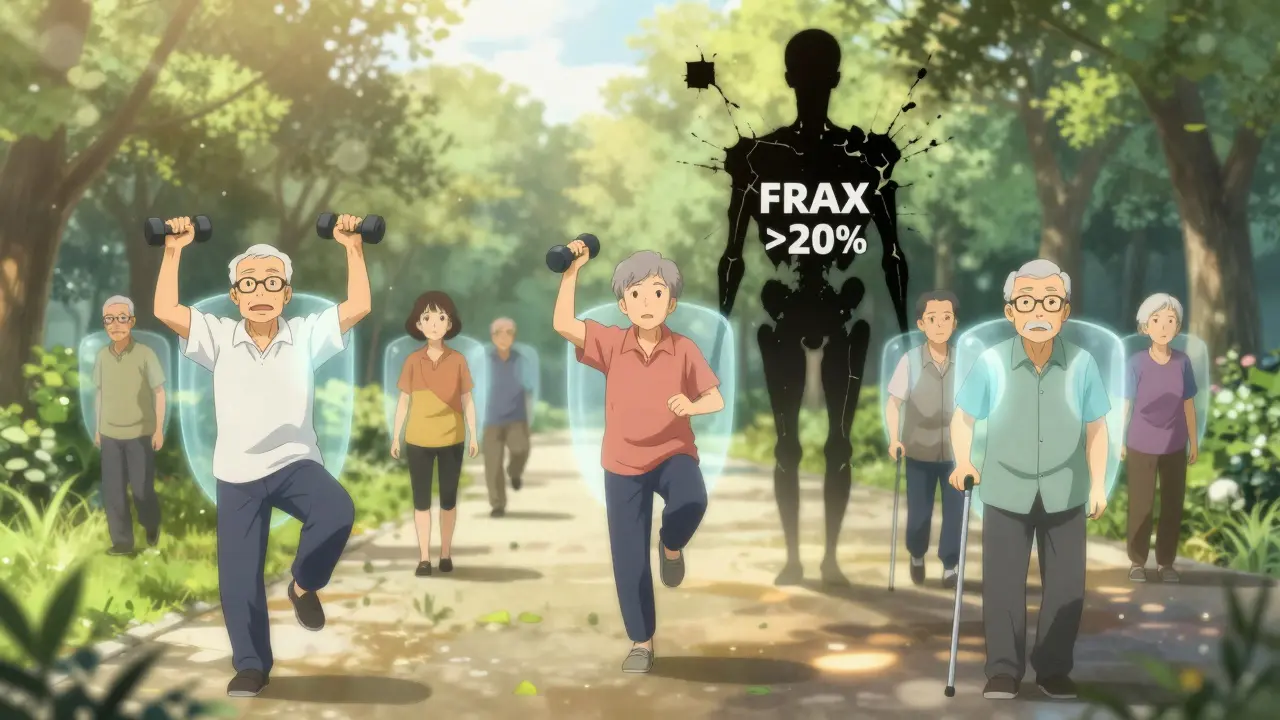
Who Really Needs This? A Practical Guide
Not everyone needs supplements or meds. Here’s who does:
- Women over 65 - automatically screen for osteoporosis.
- Men over 70 - bone loss happens here too, but it’s often ignored.
- Anyone who’s had a fragility fracture - breaking a bone from a fall from standing height or less means you have osteoporosis until proven otherwise.
- People on long-term steroids - like prednisone for asthma or arthritis - even low doses for more than 3 months.
- Those with low vitamin D levels - under 20 ng/mL. Supplement with 50,000 IU weekly for 8-12 weeks, then 800-2,000 IU daily.
- People with low calcium intake - less than 700 mg per day from food.
For everyone else - healthy, active, eating well, with normal bone density - extra calcium and vitamin D pills won’t help. Focus on weight-bearing exercise, avoiding falls, and getting sunlight. Your bones don’t need a pill. They need movement.
What to Do Right Now
Don’t wait for a fracture. Here’s your action plan:
- Get tested. Ask your doctor for a 25-hydroxyvitamin D blood test and a DEXA scan if you’re over 65 or have risk factors.
- Check your intake. Track your calcium for three days. Are you getting at least 700 mg from food? If not, add dairy, fortified plant milk, or sardines.
- Choose the right dose. If you’re deficient or at risk, take 800-1,000 IU vitamin D3 and 1,000-1,200 mg calcium daily - split into two doses.
- Consider meds if needed. If your FRAX® score is over 20%, talk to your doctor about bisphosphonates, denosumab, or anabolic agents. Don’t delay.
- Stop the myths. Vitamin D isn’t a cure-all. Calcium pills aren’t harmless. And no supplement replaces a healthy diet, exercise, or medical treatment.
Fracture prevention isn’t about popping pills. It’s about knowing your risk, using the right tools, and staying consistent. The science is clear. The tools exist. What matters now is acting before your next fall.



Comments
Skye Kooyman
January 27, 2026 AT 15:49This is the most clear-headed breakdown of bone health I've read in years. No fluff, just data.
Karen Droege
January 28, 2026 AT 11:31I've been telling my elderly patients this for a decade. Supplements are a Band-Aid. The real game-changer is DEXA scans and knowing your FRAX score. If you're over 65 and haven't had one, you're gambling with your mobility. And yes - calcium pills can give you kidney stones if you're not careful. Food first. Always.
Peter Sharplin
January 30, 2026 AT 08:58The bit about bisphosphonates and drug holidays is critical. I had a patient who took alendronate for 7 years, then stopped cold because she 'felt fine.' Ended up with an atypical femur fracture on vacation. She's now on denosumab and terrified of missing a dose. This isn't a set-it-and-forget-it situation.
Kipper Pickens
January 31, 2026 AT 18:51The pharmacokinetics of vitamin D3 absorption are non-linear and highly dependent on adipose tissue distribution and CYP2R1 polymorphisms. Most over-the-counter formulations lack bioavailability optimization, which explains the disconnect between serum levels and clinical outcomes in normovitaminotic populations. Also, the RECORD trial's power was compromised by non-adherence rates exceeding 40%.
Dan Nichols
February 1, 2026 AT 20:37You say calcium supplements increase heart attack risk? That's from a meta-analysis that didn't control for statin use or baseline inflammation markers. And you blame the pills, not the fact that people taking them are usually sedentary, diabetic, and eating processed food. Fix the lifestyle, not the supplement.
Rakesh Kakkad
February 2, 2026 AT 20:10In India, most elderly get less than 500mg calcium daily from diet. Milk is expensive, spinach is not enough. We need affordable fortified foods, not just blood tests. Also, why is everyone ignoring vitamin K2? It directs calcium to bones, not arteries. This article misses the full picture.
Allie Lehto
February 3, 2026 AT 11:23I've been taking 5000 IU of D3 daily for 3 years and my bones are stronger than my 30-year-old son's. Also, I don't trust doctors who push meds. Natural is better. I eat bone broth, walk barefoot, and sunbathe. No pills needed. You're all just selling fear.
Faisal Mohamed
February 3, 2026 AT 19:43The existential paradox of bone health: we fracture because we fear falling, yet we become immobile because we fear fracturing. The pharmaceutical industry profits from this loop. But what if the real solution isn't more drugs, but more community - sidewalks with handrails, public benches, intergenerational walking clubs? We treat bones like machines, not living tissue embedded in social ecosystems.
eric fert
February 4, 2026 AT 13:58Let’s be real. This whole bone health industry is built on fear. Who benefits? Pharma. Who loses? People who are told they’re broken before they even feel pain. I’m 72. I’ve never had a fracture. I don’t take calcium. I don’t take vitamin D. I eat meat, drink coffee, and lift my grandkids. The studies? Funded by companies that sell the pills. The real risk? Being medicated into a zombie because someone’s profit margin depends on you believing you’re deficient.
Suresh Kumar Govindan
February 6, 2026 AT 02:09The 16% hip fracture reduction with calcium + D3 is statistically significant but clinically negligible. NNT = 63. That means 63 people must take supplements for 6 years to prevent one fracture. Meanwhile, the risk of kidney stones is 17%. This is not prevention. It's medical overreach disguised as science.