GMP for Generics: FDA Requirements for Manufacturing
When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. That’s not luck. It’s the result of strict CGMP rules enforced by the FDA. These aren’t suggestions-they’re legal requirements that every generic drug maker must follow to keep selling their products in the U.S.
What Exactly Is CGMP?
CGMP stands for Current Good Manufacturing Practices. The "current" part is key. It means manufacturers can’t rely on old methods or outdated equipment. They have to use the best available technology and processes to make sure every batch of medicine is safe, pure, and effective. These rules are written into federal law under 21 CFR Parts 210 and 211. They apply equally to brand-name drugs and generics. There’s no separate standard for generics. If you’re making a generic version of a drug, you must meet the same bar as the original maker.The FDA doesn’t just check paperwork. They send inspectors into factories-domestic and foreign-to see if the rules are being followed on the ground. A single violation can lead to a warning letter, a product recall, or even a ban on selling the drug. In 2022, over 60% of all FDA warning letters for drug manufacturing went to foreign facilities, many of which produce generic drugs.
The Core Rules: What Manufacturers Must Do
The FDA’s CGMP rules cover every step of making a drug. Here’s what’s required:- Written procedures: Every single step-mixing ingredients, filling capsules, labeling bottles-must be documented. No improvising.
- Qualified staff: Employees must be trained and proven competent. Training records are checked during inspections.
- Controlled environment: Clean rooms, air filters, and humidity controls are mandatory to prevent contamination. Even tiny particles or microbes can ruin a batch.
- Equipment maintenance: Machines must be cleaned, calibrated, and serviced on schedule. Logs are kept for every action.
- Component testing: Every batch of active ingredient (API) and excipient must be tested before use. No exceptions.
- Process validation: Manufacturers must prove their process consistently produces the right product. Most use three consecutive successful batches to show this.
- Label accuracy: Labels must match the approved specification. A wrong dose or wrong name can be deadly.
- Stability testing: Drugs are stored under different conditions for months or years to make sure they don’t break down before expiration.
- Record keeping: Every record-test results, maintenance logs, training logs-must be kept for at least one year after the drug expires.
One of the most important parts is the Quality Unit. This team has real power. They can stop production, reject batches, and shut down operations if something’s wrong. No manager can override them. This structure prevents pressure to cut corners.
High-Risk Ingredients and Recent FDA Actions
Some ingredients are more dangerous than others. In May 2023, the FDA issued an immediate guidance requiring all manufacturers to test high-risk components like glycerin and sorbitol for toxic contaminants like diethylene glycol and ethylene glycol. This wasn’t theoretical. In 2022, contaminated cough syrups from Pakistan caused over 70 child deaths. The root cause? A supplier skipped basic testing because it was cheaper.That’s why the FDA now demands proof of testing for these high-risk materials-even if they’re not the active ingredient. Generic drug makers can’t just trust their suppliers. They have to verify it themselves.
What Happens When Companies Fail
In 2022, 12 generic metformin products were recalled because of NDMA contamination-a probable carcinogen. The FDA’s investigation found the manufacturers didn’t validate their cleaning procedures between batches. One company even altered test results to hide the problem. That’s a data integrity violation, one of the most serious offenses under CGMP.Warning letters are public. Companies that ignore them risk import bans. In 2023, the FDA blocked shipments from over 100 foreign facilities for CGMP violations. Many of these were generic drug makers in India and China.
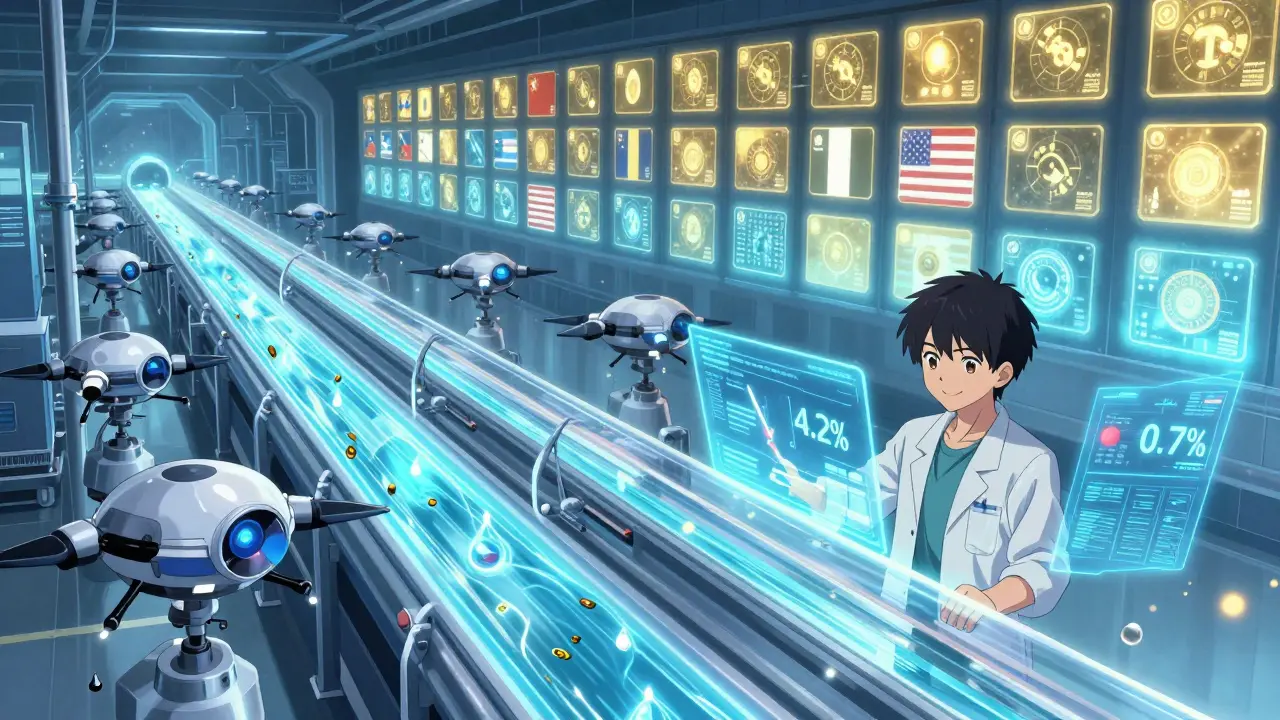
But it’s not all bad news. Teva, a major generic manufacturer, switched to continuous manufacturing for a heart medication. Instead of making drugs in batches, they now produce them in a steady flow. This cut batch failures from 4.2% to 0.7%-all while staying fully compliant with CGMP. It’s proof that modern tech can make quality better, not harder.
Costs and Challenges for Manufacturers
Meeting CGMP isn’t cheap. For a mid-sized generic company, annual compliance costs average $2.3 million. That’s about 12-15% of total manufacturing expenses. Small companies struggle the most. One Reddit user shared how implementing electronic batch records-a requirement under 21 CFR Part 11-cost $1.2 million and took 14 months for a 50-person facility.Documentation is the biggest headache. Over 68% of manufacturers say keeping records is the hardest part. Inspectors look for audit trails, timestamps, and proof that no one altered data. Many companies still use paper logs, which are easy to tamper with. Switching to electronic systems is expensive but necessary.
Another issue? Inconsistent inspections. A 2023 survey found that 57% of manufacturers felt different FDA inspectors interpreted the rules differently. One inspector might flag a minor record gap. Another might ignore it. That unpredictability adds stress and cost.
How the Industry Is Changing
The FDA is pushing for modernization. Their 2023-2027 plan includes:- 25% more inspections of foreign facilities
- Stronger focus on data integrity (Part 11 compliance)
- Guidance for continuous manufacturing (draft expected in 2024)
- Stricter supply chain controls under the Drug Supply Chain Security Act
More companies are adopting AI and predictive analytics to catch quality issues before they happen. By 2028, 65% of manufacturers are expected to use these tools. That’s a big shift from reactive testing to real-time quality control.
Still, adoption of advanced tech is slow. Only 18% of generic manufacturing facilities use continuous manufacturing or automation. Why? Because validating new systems under CGMP is complex and time-consuming. Many small firms don’t have the resources.
Why This Matters to You
You don’t need to know the details of 21 CFR Part 211. But you should know this: the generic drug you take is held to the same standard as the brand-name version. The FDA doesn’t cut corners. If a generic drug is on the market, it’s because the FDA has seen proof it’s safe and effective.When you see a price drop, don’t assume quality dropped too. The savings come from lower marketing costs and competition-not from cutting corners on safety. CGMP is the reason you can trust a $5 generic instead of a $100 brand-name pill.
But trust isn’t blind. The FDA’s job is to keep that trust. And when they find problems, they act. That’s why recalls happen. That’s why inspections continue. That’s why the system works.
What’s Next for Generic Drug Manufacturing
The future of generics isn’t just about cheaper pills. It’s about smarter, safer production. The FDA is moving toward real-time quality monitoring. Imagine a machine that detects a contamination risk before a single pill is made. That’s the goal.Supply chain security is another big focus. After pandemic-related shortages, the FDA is demanding better tracking of active ingredients. You’ll see more manufacturers testing raw materials at multiple points-not just at the start.
International standards are also aligning. The FDA and Europe’s EMA now share 85% of the same GMP rules. But the FDA still demands more documentation and more frequent checks. That’s a cost-but it’s also a guarantee.
For patients, that means more confidence. For manufacturers, it means higher barriers to entry. But for the system as a whole, it means safer medicine for everyone.
Are generic drugs held to the same quality standards as brand-name drugs?
Yes. The FDA requires that generic drugs be manufactured under the same Current Good Manufacturing Practices (CGMP) as brand-name drugs. There is no separate or lower standard for generics. Every batch must meet identical requirements for identity, strength, purity, and quality.
What happens if a generic drug manufacturer violates CGMP rules?
Violations can lead to warning letters, import alerts, product recalls, or even a ban on selling the drug. The FDA can shut down production until the issues are fixed. In serious cases, companies face civil penalties or criminal charges. For example, in 2022, 12 generic metformin products were recalled due to inadequate process controls and falsified data.
How often does the FDA inspect generic drug facilities?
Domestic facilities are inspected about every 18-24 months on average, with some receiving inspections more frequently based on risk. Foreign facilities are inspected less often due to logistics, but the FDA is increasing foreign inspections by 25% through 2027. In 2022, 63% of all data integrity warning letters went to foreign facilities.
Why are CGMP compliance costs so high for small generic manufacturers?
Small manufacturers face fixed costs like facility qualification, electronic record systems, staff training, and validation testing that don’t scale down. A mid-sized company spends an average of $2.3 million annually on compliance. Implementing FDA-compliant electronic systems can cost over $1 million and take over a year-costs that are harder to absorb with smaller profit margins.
Can a generic drug be approved without CGMP compliance?
No. The FDA reviews CGMP compliance as part of every Abbreviated New Drug Application (ANDA). A facility must pass a pre-approval inspection before the drug can be approved. If the inspection finds major violations, the application is denied. Even after approval, ongoing compliance is required to keep selling the drug.
What are the biggest CGMP challenges facing generic manufacturers today?
The top challenges are data integrity (especially under 21 CFR Part 11), inconsistent FDA inspection interpretations, supply chain verification for raw materials, and the cost of modernizing equipment. Over 78% of manufacturers report difficulties with audit trails, and 43% have experienced component testing failures in recent years.





