How to Time Your Medications to Avoid Dangerous Drug Interactions
Every year, thousands of people end up in the hospital not because their medication stopped working, but because they took it at the wrong time. It’s not always about taking too much or the wrong pill-it’s about when you take it. Timing your medications properly can prevent dangerous interactions, keep your treatment effective, and even save your life. Yet most people don’t know this is even an issue.
Why Timing Matters More Than You Think
Not all drug interactions are the same. Some happen because two drugs clash chemically in your bloodstream. Others happen because one drug blocks another from being absorbed in your gut. The second kind? That’s where timing saves the day. For example, if you take an antibiotic like ciprofloxacin with an antacid like Tums, the calcium and magnesium in the antacid can bind to the antibiotic and stop it from working. Studies show this can cut absorption by up to 90%. But if you wait just two hours between them? The antibiotic works fine. Same goes for levothyroxine, the thyroid medication millions take daily. If you take it with iron, calcium, or even coffee, your body absorbs barely half of it. Wait four hours, and you get nearly all of it. This isn’t theoretical. In a 2021 trial at UCSF Medical Center, pharmacists started timing iron supplements and proton pump inhibitors (like omeprazole) four hours apart in elderly patients. Within 18 months, cases of iron-deficiency anemia dropped by 32%. That’s not luck-it’s science.Which Interactions Can Be Fixed by Timing?
Only certain types of interactions respond to timing. The big winners are those that affect absorption in your stomach or intestines. Here are the most common ones:- Antibiotics + Antacids/Calcium/Iron: Fluoroquinolones (ciprofloxacin, levofloxacin), tetracyclines (doxycycline), and some sulfonamides need at least 2-3 hours between them and calcium, iron, magnesium, or aluminum products. That includes multivitamins, supplements, and even dairy.
- Thyroid meds + Supplements: Levothyroxine must be taken on an empty stomach, at least 4 hours before or after iron, calcium, soy, or fiber supplements. Even coffee can interfere-wait 30-60 minutes after taking it.
- Bisphosphonates + Food: Alendronate (Fosamax) and similar osteoporosis drugs need to be taken with a full glass of water, first thing in the morning, and you must wait 30 minutes before eating, drinking, or taking anything else.
- Statins + Grapefruit: While this isn’t about timing, grapefruit juice can permanently block enzymes that break down some statins (like simvastatin). You can’t just wait-it’s safer to avoid it completely.
What Happens When You Ignore Timing?
Ignoring these windows isn’t just risky-it’s common. A 2022 survey of older adults on 10 or more medications found that 40% didn’t follow their timing instructions. Why? Because the instructions are confusing. “I was told to take my thyroid pill in the morning, my calcium at lunch, and my iron at night,” said Carol, 72, from Ohio. “But I’d forget which one needed space. Sometimes I’d take them all together just to get it over with.” The result? She developed severe fatigue and hair loss. Her doctor finally realized her levothyroxine wasn’t being absorbed. Once she started spacing her calcium and iron by four hours, her TSH levels normalized in six weeks. In hospitals, nurses spend 12-15 minutes per patient every day just coordinating when to give each pill. In outpatient clinics, where there’s no staff to help, patients are left to figure it out themselves. And that’s where things fall apart.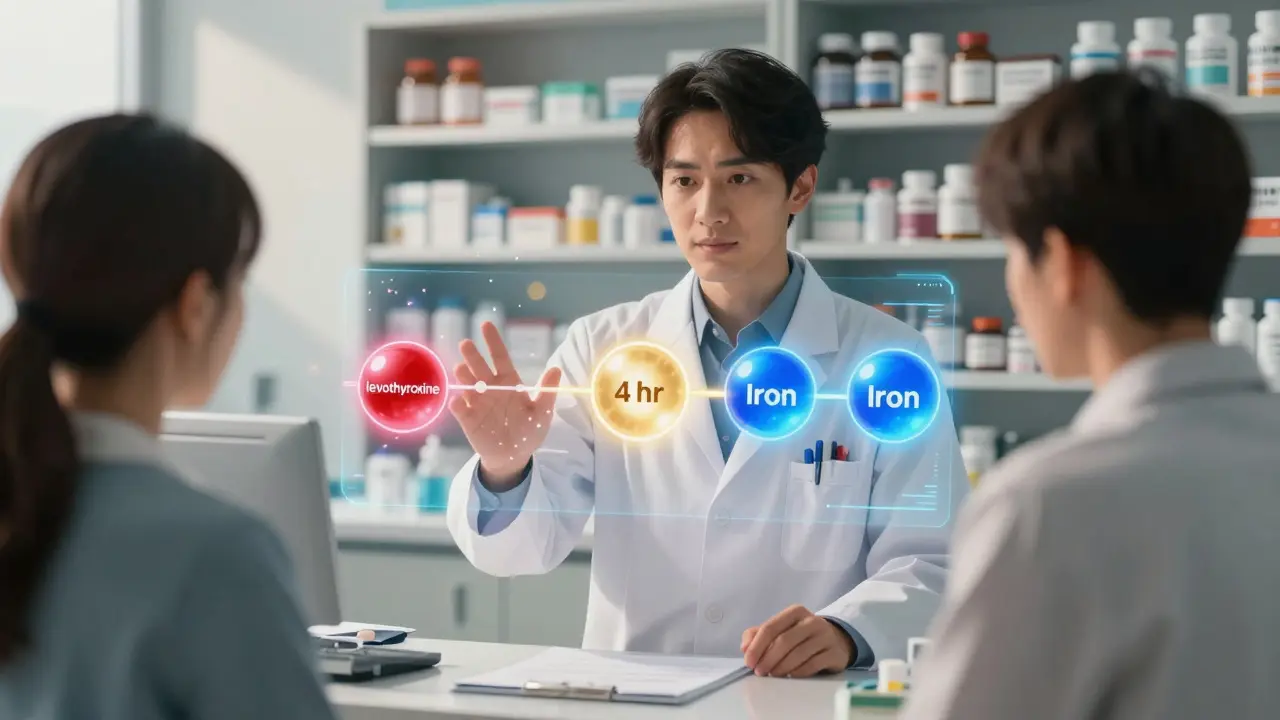
How to Get Your Timing Right
You don’t need to memorize every interaction. Here’s how to make it simple:- Do a full med review. Write down every pill, supplement, and OTC drug you take-including what time you take them. Bring this to your doctor or pharmacist at least once a year.
- Ask: “Does any of this need spacing?” Don’t assume your doctor knows. Ask specifically about absorption-based interactions. Mention any supplements you take.
- Use a reliable source. Look up your drugs in Lexicomp, Micromedex, or the FDA’s drug interaction database. If you’re not sure, call your pharmacist-they’re trained for this.
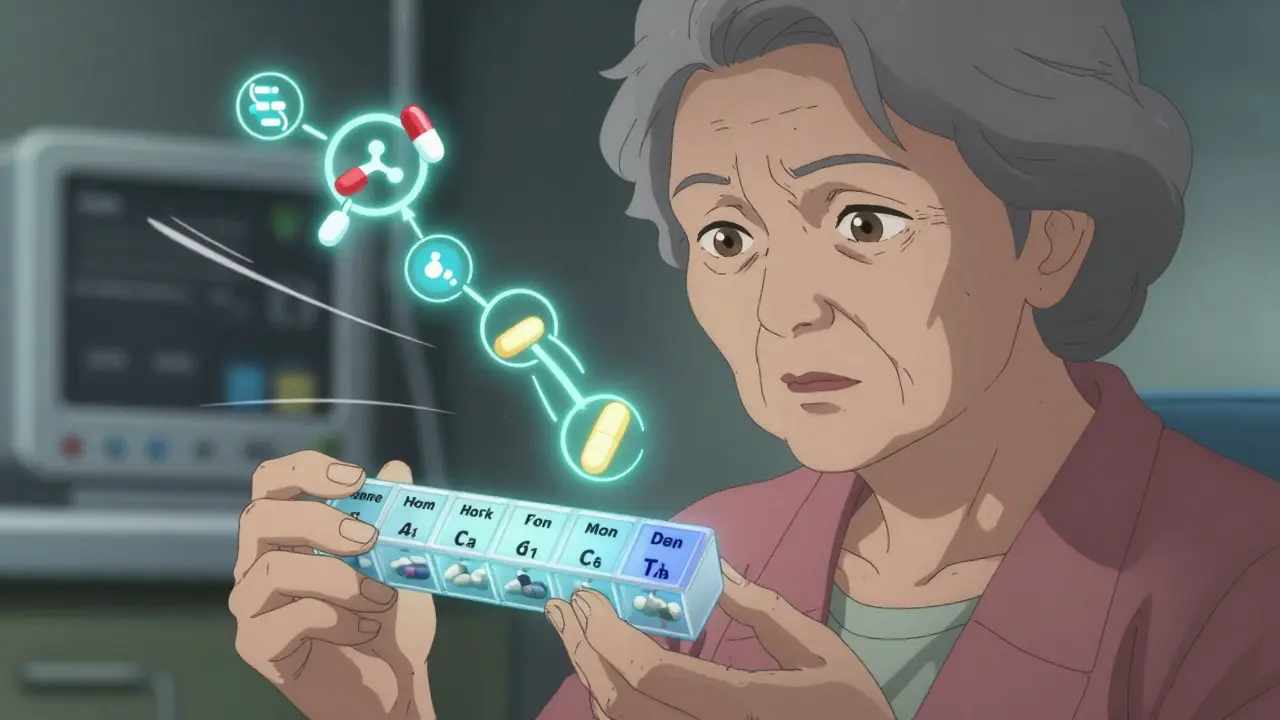
- Build a schedule. Use a pill organizer with separate compartments for morning, afternoon, evening, and night. Label each section clearly. Some even have alarms.
- Use a digital reminder. Apps like Medisafe or MyTherapy let you set custom alerts with notes like “Wait 4 hours before calcium.” One 2021 study showed these apps improved timing adherence by 57%.
What Works Best in Real Life
The most successful systems don’t rely on patients remembering everything. They use tools:- Pill organizers with time slots: Reduces timing errors by 43%, according to the Agency for Healthcare Research and Quality.
- Electronic health records with alerts: Hospitals like Kaiser Permanente use CPOE systems that flag potential timing conflicts. Since 2022, they’ve cut drug-interaction hospitalizations by 29%.
- Pharmacist-led medication therapy management: Many insurance plans now cover this service. A pharmacist sits down with you, reviews all your meds, and builds a personalized schedule. It takes 25-30 minutes, but it’s free with many plans.

What Doesn’t Work
Don’t rely on:- Memory alone. Even smart people forget. A 2023 study found that 68% of patients over 65 couldn’t correctly recall their own timing instructions.
- Assuming “once a day” means any time. If your pill says “take daily,” that doesn’t mean “whenever you remember.” Some meds need to be taken at the same time every day to work properly.
- Skipping doses to avoid conflict. If your thyroid med and iron clash, don’t skip the thyroid pill. That can cause serious problems. Space them out instead.
When to Call Your Doctor
If you notice any of these after changing your timing:- Your symptoms return or get worse
- You feel unusually tired, dizzy, or nauseous
- You have unexplained bruising or bleeding
- Your blood pressure, heart rate, or blood sugar changes without reason
Final Thoughts: Timing Is a Tool, Not a Trick
You don’t have to choose between taking your life-saving meds and staying safe. Timing gives you both. It’s not complicated-it’s just overlooked. The FDA now recommends time separation for 17 high-risk drug pairs. That’s a big shift. But real change only happens when patients and providers work together. Start small. Pick one medication you take daily. Check if it interacts with anything else. Space them out. Track how you feel. You might be surprised how much better you feel just by changing the clock.Can I take my vitamins with my prescription drugs?
It depends. Calcium, iron, magnesium, and zinc can block absorption of antibiotics like ciprofloxacin and doxycycline, as well as thyroid medication. Wait at least 2-4 hours between these. Multivitamins often contain these minerals, so check the label. If you’re unsure, take your vitamins at night and your meds in the morning.
Is it okay to take my pills with food?
Some meds need an empty stomach, others need food. Levothyroxine, bisphosphonates, and some antibiotics must be taken on an empty stomach-wait 30-60 minutes before eating. Others, like statins or certain blood pressure pills, work better with food. Always check the label or ask your pharmacist.
What if I forget to space my medications?
If you accidentally take two interacting drugs close together, don’t panic. Skip the next dose of one if it’s safe to do so (check with your pharmacist). Don’t double up later. Going forward, use a pill organizer or app to avoid repeats. One missed spacing won’t cause harm-but repeated mistakes can reduce effectiveness over time.
Do over-the-counter drugs cause timing issues too?
Yes. Antacids, cold medicines with iron or calcium, and even some herbal supplements like St. John’s wort can interfere. St. John’s wort, for example, speeds up how fast your body breaks down antidepressants and birth control. That’s a metabolic interaction-timing won’t fix it. You’ll need to stop the herb or switch meds.
How do I know if my meds are working properly?
Your doctor can order blood tests to check levels. For thyroid meds, that’s TSH and free T4. For warfarin, it’s INR. For antibiotics, symptoms should improve within a few days. If you’re feeling worse or no better after a week, timing may be the issue. Ask for a review of your schedule.






Comments
Angela Goree
January 3, 2026 AT 21:04Who the hell lets their pharmacist or doctor just hand them a list of 12 pills and say ‘take them whenever’? This is criminal negligence. I’ve seen grandmas on 17 meds taking everything at breakfast like it’s a buffet. No wonder half of them end up in the ER. Someone needs to get sued over this.
erica yabut
January 4, 2026 AT 15:59How delightfully bourgeois of you to assume that people have the luxury of time, pill organizers, and access to Lexicomp. My grandmother takes her meds with her coffee because she’s 84, has no family, and works two shifts at Walmart. You’re not educating-you’re shaming. This isn’t a TED Talk, it’s a survival manual for the working poor.
Vincent Sunio
January 5, 2026 AT 15:59The author’s conflation of pharmacokinetic interactions with pharmacodynamic ones is scientifically incoherent. While temporal separation mitigates absorption-based interference, it does nothing to alter enzyme inhibition or induction. The piece exhibits a dangerous oversimplification of clinical pharmacology, which may lead to misplaced confidence in non-pharmacologic interventions for high-risk drug pairs. A more rigorous citation of the FDA’s 2023 guidance on time-dependent interactions would have been preferable.
Shanahan Crowell
January 6, 2026 AT 23:06Y’know what? This changed my life. I used to take my thyroid pill with my protein shake-no wonder I was exhausted all the time. I started waiting 45 minutes, now I have energy, my hair’s growing back, and I’m not crying in the shower every morning. It’s not magic-it’s just listening. Thank you for saying what no one else did.
Kerry Howarth
January 8, 2026 AT 09:44One change. One habit. That’s all it takes. Start with your thyroid med or your antibiotic. Space it out. Track how you feel for a week. You don’t need an app or a pillbox-just a clock and a little discipline. Small wins build big results.
Tiffany Channell
January 8, 2026 AT 22:27Let’s be real-this is all a pharmaceutical industry ploy to sell more pill organizers and apps. The real issue? Doctors don’t coordinate care. They prescribe like they’re playing Jenga. And now we’re supposed to become our own pharmacists? No thanks. I’ll keep taking my pills whenever I remember and let the chips fall where they may.
Joy F
January 9, 2026 AT 07:22Think about it: we live in a world where we can summon a car with a tap, but we’re expected to remember that calcium steals the spotlight from ciprofloxacin like some tragic Shakespearean betrayal. Our bodies are not vending machines. We are not machines. We are fragile, beautiful, forgetful creatures drowning in a sea of prescriptions. The real tragedy isn’t the interaction-it’s that we’ve been abandoned by the system that promised to care for us.
Haley Parizo
January 10, 2026 AT 22:48I’ve been taking my levothyroxine with coffee for 8 years. I’ve also been traveling to 12 countries, speaking five languages, and writing three novels. If I can do all that on ‘suboptimal absorption,’ then maybe the problem isn’t me-it’s the medical industrial complex trying to pathologize human imperfection. Let people live. Let them drink their coffee.
Ian Detrick
January 12, 2026 AT 15:07There’s wisdom here. Not just medical-human. We’ve turned healthcare into a checklist, not a conversation. But timing? That’s rhythm. That’s listening to your body, your schedule, your life. It’s not about perfection. It’s about awareness. And awareness is the first step toward reclaiming your health.
Angela Fisher
January 14, 2026 AT 11:40Did you know the FDA is secretly working with Big Pharma to make people dependent on pill organizers? They know if you take your meds right, you won’t need as many drugs. So they bury this info under 10 pages of jargon. And now they want you to buy an app? I’ve seen the documents. They’re coded. The ‘4-hour rule’? It’s not science-it’s a distraction. They want you distracted while they raise prices on insulin. Don’t fall for it.
Neela Sharma
January 15, 2026 AT 14:19In India, we call this ‘timing ka khel’-the game of timing. My aunt takes her BP pill with breakfast, her iron after lunch, and her thyroid at dawn. She doesn’t have an app. She has a calendar on her wall with red dots. She’s 78. Still walks two miles a day. Simple. Human. No fancy tech. Just love and routine.
Shruti Badhwar
January 17, 2026 AT 10:14While the article presents compelling clinical evidence, it neglects to address socioeconomic disparities in medication adherence. The proposed solutions-pill organizers, digital reminders, pharmacist consultations-are inaccessible to low-income populations without smartphones, stable housing, or insurance coverage. A public health framework must precede individual behavioral interventions.
Brittany Wallace
January 18, 2026 AT 04:18My dad took his blood pressure med with grapefruit juice for 12 years. He didn’t know it was dangerous. Then one day, he passed out in the kitchen. Now he takes it with water, at 7 a.m., every day. No app. Just us reminding him. It’s not about being perfect. It’s about being together. That’s the real medicine.