Statins and Antifungal Medications: What You Need to Know About Rhabdomyolysis Risk

Statin-Antifungal Interaction Risk Checker
Risk Assessment Tool
Risk Assessment Results
Important Safety Information
Do not take this tool as medical advice. Always consult your doctor or pharmacist before changing medications.
Severe muscle pain, dark urine, or weakness require immediate medical attention.
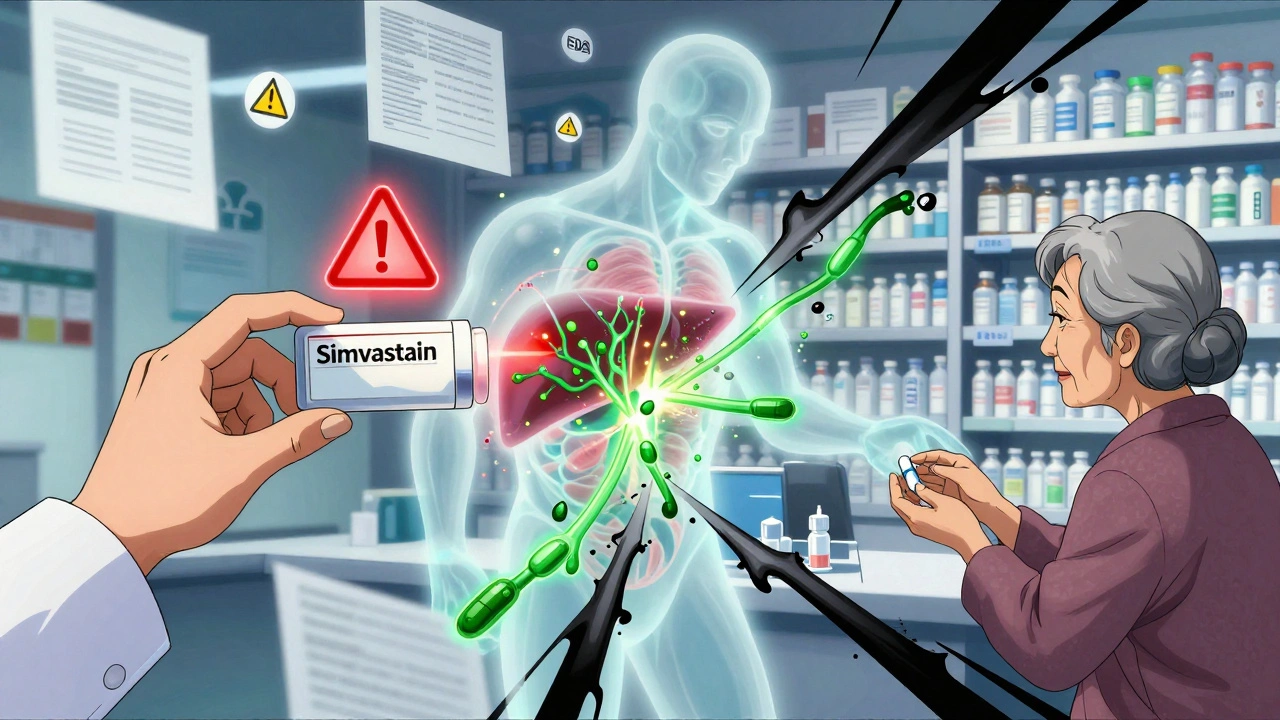
Imagine you’re taking a statin to lower your cholesterol, and then you get a fungal infection-maybe athlete’s foot, a yeast infection, or a stubborn nail fungus. Your doctor prescribes an antifungal like fluconazole or itraconazole. Sounds simple, right? But here’s the hidden danger: statins and certain antifungals can combine to trigger a life-threatening condition called rhabdomyolysis. This isn’t a rare theory-it’s a documented, preventable emergency that shows up in hospitals every year.
Why This Interaction Happens
Statins work by blocking an enzyme in your liver that makes cholesterol. But your body doesn’t just flush them out after they do their job. Most statins are broken down by a group of liver enzymes called CYP3A4. That’s where antifungals come in. Azole antifungals-like ketoconazole, itraconazole, voriconazole, and even fluconazole at high doses-shut down CYP3A4 like a switch. When that happens, your statin doesn’t get cleared from your system. It builds up. And when it builds up too much, it starts tearing apart your muscle cells.This isn’t just theory. In 2012, the FDA updated warnings after reviewing hundreds of cases. They found that combining simvastatin with itraconazole could increase simvastatin levels by more than 10 times. That’s not a typo. Ten times. One study showed that a single 40 mg dose of simvastatin with itraconazole spiked blood levels to the equivalent of 400 mg. That’s a massive overdose.
Which Statins Are Riskiest?
Not all statins are created equal when it comes to this interaction. Some are like gasoline near a spark. Others are practically fireproof.- High risk: Simvastatin, lovastatin, and atorvastatin. These rely heavily on CYP3A4 to break down. Simvastatin is the worst offender. Even a 20 mg dose can become dangerous with a strong antifungal.
- Moderate risk: Pitavastatin and rosuvastatin. These use CYP3A4 a little, but also have other clearance paths. Still, caution is needed-especially with voriconazole.
- Low risk: Pravastatin, fluvastatin, and rosuvastatin (at lower doses). These mostly bypass CYP3A4. Pravastatin, for example, is cleared by the kidneys, not the liver. That’s why doctors often switch patients to it when antifungals are needed.
Here’s what the numbers look like in real-world terms:
| Statin | Antifungal | Increased Exposure | Risk Level |
|---|---|---|---|
| Simvastatin | Itraconazole | 1,160% | Extreme |
| Simvastatin | Fluconazole (400 mg/day) | 350% | High |
| Atorvastatin | Itraconazole | 360% | High |
| Atorvastatin | Fluconazole (200 mg/day) | 80% | Moderate |
| Pravastatin | Any azole | 0-10% | Low |
| Fluvastatin | Fluconazole | 10-15% | Low |
What Rhabdomyolysis Actually Feels Like
Rhabdomyolysis isn’t just muscle soreness after a tough workout. It’s your muscles literally breaking down. The muscle cells leak a protein called myoglobin into your blood. That stuff clogs your kidneys. If it’s not caught fast, you can end up in the ICU with kidney failure.People who’ve been through it describe it like this:
- Severe, unexplained muscle pain-worse than any cramp, feels like your muscles are being crushed.
- Weakness so bad you can’t stand up from a chair or climb stairs.
- Dark urine-brown, tea-colored, or even cola-colored. That’s myoglobin being flushed out.
- Fever, nausea, confusion. Sometimes it looks like the flu.
A 2018 case report in Pharmacotherapy described a 68-year-old man who took simvastatin 40 mg and fluconazole 200 mg for a toenail fungus. Seven days later, his creatine kinase (CK) level hit 18,400 U/L. Normal is 30-200. He spent three days in the hospital. He didn’t die-but he came close.
And this isn’t rare. Between 2010 and 2019, over 1,200 cases of rhabdomyolysis linked to statin-azole combinations were reported to the FDA. Simvastatin with itraconazole made up nearly 40% of those cases. Fluconazole with simvastatin was second.
Who’s Most at Risk?
It’s not just about the drugs. Your body matters too.- Age 65+: Liver and kidney function slow down. Your body can’t clear drugs as fast.
- Chronic kidney disease: Even if you’re on a low-risk statin, poor kidney function makes toxicity more likely.
- Diabetes or hypothyroidism: These conditions make muscles more sensitive to statin damage.
- Multiple medications: If you’re also on blood pressure meds, antibiotics like clarithromycin, or even grapefruit juice, the risk stacks up.
- Genetics: Some people have a gene variant (CYP3A5*3/*3) that makes them poor metabolizers. They’re 2.3 times more likely to have a bad reaction.
One 2022 study found that 23.4% of patients over 75 got a contraindicated statin-azole combo-even with all the warnings out there.
What Doctors Should Do
Good doctors don’t just write prescriptions. They check for traps.The safest move? Stop simvastatin and lovastatin completely while taking strong antifungals like itraconazole, ketoconazole, or voriconazole. Don’t just lower the dose-stop it. Restart the statin only 2-3 days after the antifungal is done.
If you need an antifungal and you’re on statins, here’s what works:
- Switch to pravastatin (40 mg daily). It’s safe with all azoles.
- Use fluvastatin (80 mg daily). It’s metabolized by a different enzyme.
- Try rosuvastatin (max 20 mg daily). Low risk, but monitor.
- Consider isavuconazole as the antifungal. It doesn’t block CYP3A4. It’s newer, pricier, but safer if you need long-term treatment.
For moderate inhibitors like fluconazole (200 mg or less), guidelines say:
- Simvastatin: Max 10 mg daily
- Atorvastatin: Max 20 mg daily
- Pravastatin, fluvastatin, rosuvastatin: No dose limits needed

What You Can Do
You’re not powerless. If you’re on a statin and your doctor prescribes an antifungal, ask these questions:- Which statin am I on? Is it simvastatin, lovastatin, or atorvastatin?
- Is this antifungal a strong CYP3A4 inhibitor? (Ketoconazole, itraconazole, voriconazole = yes. Fluconazole = maybe, if it’s 200 mg or more.)
- Can I switch to pravastatin or fluvastatin while I’m on this antifungal?
- Should I get a baseline CK test before starting?
- What symptoms should I watch for? When do I call you immediately?
Don’t assume your pharmacist caught it. Don’t assume your doctor remembered. Double-check. Bring a list of all your meds-prescription, OTC, supplements. That’s how you protect yourself.
Technology Is Helping
Hospitals are finally catching on. Electronic health records like Epic now have hard stops. If a doctor tries to prescribe simvastatin 40 mg with itraconazole, the system won’t let them. It pops up a warning. At Mayo Clinic, this cut dangerous prescriptions by 87%.But in outpatient clinics? Still a problem. Many community pharmacies don’t have the same alerts. That’s why you have to be your own advocate.
The Bigger Picture
This isn’t just about one drug pair. It’s about how medicine still treats prescriptions like puzzle pieces you can snap together without checking for sharp edges. Statins are among the most prescribed drugs in the world. Antifungals are common, especially in older adults with diabetes or poor circulation. Millions of people are at risk.But here’s the good news: this is one of the most preventable drug reactions out there. We know exactly which combinations kill. We know how to avoid them. We’ve had the data for over a decade.
What’s missing isn’t science. It’s awareness. And action.
If you’re taking a statin and need an antifungal, don’t wait for symptoms. Ask the questions before you fill the prescription. Your muscles-and your kidneys-will thank you.






Comments
Christian Landry
December 10, 2025 AT 17:59Holy crap, I had no idea fluconazole could do this to statins. I was on simvastatin for my cholesterol and took it for a yeast infection last year... luckily I just had mild muscle soreness. But now I’m freaked out. 😅
Katie Harrison
December 11, 2025 AT 23:05This is exactly why I always print out my meds list and hand it to every doctor... even the dermatologist. I’ve seen too many people get confused by 'just a little antifungal'-it’s not 'just a little' when your muscles start melting. 🙏
Michael Robinson
December 13, 2025 AT 21:36So basically, your body’s cleanup crew gets blocked. The statin just sits there, getting stronger and stronger until it starts eating your muscles. It’s like leaving a gas can next to a furnace. You don’t need a PhD to get that.
Graham Abbas
December 14, 2025 AT 16:01I read this and thought-this is the kind of thing that kills people quietly. No fanfare. No headlines. Just an old man who went to the pharmacy for toenail fungus and never came home from the hospital. We treat meds like candy. We need to stop. This isn’t theoretical. It’s happening every damn day.
Haley P Law
December 15, 2025 AT 20:14I JUST got prescribed fluconazole for a yeast infection and I’m on atorvastatin. I’m gonna call my doctor right now. Like, NOW. 🤯 I don’t care if it’s 2am. I’d rather be embarrassed than in the ICU. #MedicationSafety
Andrea DeWinter
December 16, 2025 AT 20:29Pravastatin is your best friend here. Switching to it is like swapping a landmine for a rubber duck. My grandma’s on it now after her antifungal scare-no issues. And it’s cheap. Ask your doc. Seriously. It’s not hard.
Steve Sullivan
December 18, 2025 AT 13:22I’m 72. Took simvastatin for 8 years. Got fluconazole for ringworm. Felt like I got hit by a truck for a week. CK was through the roof. Docs didn’t even ask about my meds. I’m lucky I didn’t lose a kidney. 🤬 If you’re on statins and get ANY antifungal-STOP. ASK. DOUBLE CHECK. This ain’t your grandma’s medicine game anymore.
Evelyn Pastrana
December 18, 2025 AT 15:23So let me get this straight... we have a system that can block dangerous combos in big hospitals... but your local pharmacy? Still flying blind. 🤦♀️ Meanwhile, I’m supposed to be the expert on my own body? Thanks, healthcare system. I’ll just carry a white flag and a list of my pills. 🙃