Trimethoprim-Sulfamethoxazole and Warfarin: Why INR Rises and How to Stay Safe
Warfarin-TMP-SMX Risk Calculator
Your Risk Assessment
Enter your details to get a personalized risk assessment for INR elevation when taking trimethoprim-sulfamethoxazole (Bactrim/Septra) while on warfarin.
Results
Important Timing Information
INR typically starts rising within 36-72 hours of starting trimethoprim-sulfamethoxazole. Don't wait for your next scheduled blood test—get checked within 48 hours of starting this antibiotic.
When to Check Your INR
When you're on warfarin, even a simple antibiotic can throw your blood thinning off balance-sometimes dangerously so. Trimethoprim-sulfamethoxazole, sold under brand names like Bactrim or Septra, is one of the most common antibiotics prescribed for urinary tract infections, bronchitis, and skin infections. But if you're taking warfarin, this combo can cause your INR to spike, putting you at risk for serious, even life-threatening bleeding. This isn’t a rare side effect. It’s a well-documented, predictable interaction that happens in real time, often within just a couple of days.
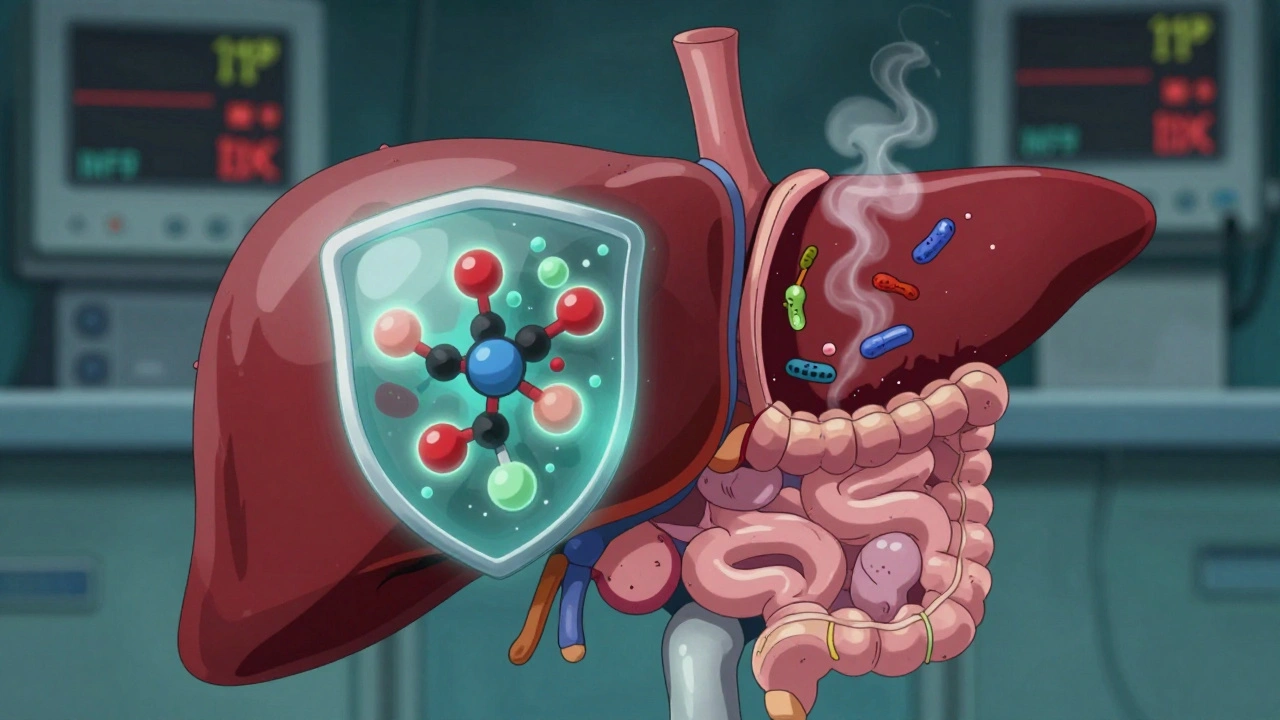
Why This Interaction Happens
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. It’s a delicate balance. Too little, and you bleed. Too much, and clots form. The drug itself is tricky: about 97-99% of it sticks tightly to proteins in your blood, mainly albumin. That leaves very little free-floating warfarin circulating-and that’s the part that actually does the work. When another drug, like trimethoprim-sulfamethoxazole, comes along and also binds tightly to those same proteins, it pushes warfarin out. Suddenly, more warfarin is free in your bloodstream, and your INR rises. But that’s not the whole story. The more potent half of warfarin, called S-warfarin, is broken down mainly by an enzyme in your liver called CYP2C9. Trimethoprim, one of the two parts of this antibiotic, blocks that enzyme. So your body can’t clear the warfarin as quickly. It builds up. Studies show this alone can reduce warfarin clearance by 20-30%. Add that to the protein displacement, and you’ve got a double punch. There’s also a third factor: your gut bacteria. Some of them make vitamin K. Trimethoprim-sulfamethoxazole kills off those bacteria. Less vitamin K means your liver can’t make clotting factors as fast, which makes warfarin’s effect stronger. It’s not the biggest player, but it adds up-especially in older adults or people with poor nutrition.How Fast Does INR Rise?
This isn’t a slow burn. Most people see their INR start climbing within 36 to 72 hours after starting the antibiotic. That’s why waiting until your next routine blood test is a dangerous mistake. One nurse practitioner in a clinical forum described seeing INR jump from 2.5 to 6.0 in just three days after a patient started Bactrim for a UTI. That’s not unusual. In fact, a 2023 study found TMP-SMX raises INR by an average of 1.8 points-more than double the effect of amoxicillin, which only bumps it up by 0.4 points. Fluoroquinolones like ciprofloxacin fall in between, raising INR by about 0.9 points. The timing matters. If you’re on warfarin and get prescribed this antibiotic, don’t wait for your next scheduled INR check. Get tested within 48 hours. That’s the window where the spike usually happens.Who’s at Highest Risk?
Not everyone reacts the same way. Some people take TMP-SMX and their INR barely budges. Others go from a stable 2.8 to 8.2 in under a week. Why? Several factors make the interaction worse:- Age over 75: Older adults clear drugs slower and often have less muscle mass and protein, which changes how warfarin behaves.
- Liver disease: Your liver handles both warfarin metabolism and protein production. If it’s damaged, the interaction gets stronger.
- Heart failure: Fluid buildup can alter how drugs are distributed in your body.
- Low vitamin K intake: If you’re not eating leafy greens or other vitamin K-rich foods, your body has less buffer against warfarin’s effects.
- Male gender: Studies show men are about 9% more likely than women to have a significant INR rise with this combo.
What Happens When INR Goes Too High?
An INR above 4.0 means your blood is taking longer to clot. That’s the red flag zone. Above 5.0, the risk of bleeding jumps sharply. And above 10? You’re in emergency territory. Real-world data from the FDA’s adverse event system shows that over five years, there were 1,842 reports of INR spikes linked to TMP-SMX. Nearly half of those cases led to hospitalization. And 68 people died from bleeding complications. Symptoms of dangerous bleeding include:- Unexplained bruising or purple spots on the skin
- Bleeding gums when brushing teeth
- Nosebleeds that won’t stop
- Red or dark brown urine
- Black, tarry stools
- Severe headaches or dizziness (possible brain bleed)
- Unusual swelling or pain in joints
What Should You Do If You Need This Antibiotic?
The short answer: avoid it if you can. But sometimes, you don’t have a choice. Maybe you have a severe infection, and other antibiotics won’t work. Here’s what to do if you must take TMP-SMX while on warfarin:- Check your INR before you start. Know your baseline.
- Get your INR checked within 48 hours. Don’t wait for your next appointment.
- Reduce your warfarin dose preemptively. In high-risk patients, doctors often cut the dose by 20-30% before starting the antibiotic. This isn’t guesswork-it’s standard protocol at major hospitals.
- Test every 3-4 days while on the antibiotic. Keep checking until at least 3 days after you stop it. The effect can linger.
- Ask for alternatives. Nitrofurantoin is a common go-to for UTIs and doesn’t interact with warfarin. Amoxicillin is another safe bet. Doxycycline and azithromycin are also low-risk options depending on the infection.
What If Your INR Is Already Too High?
If your INR is between 4.0 and 5.0 and you’re not bleeding:- Hold off on your next warfarin dose for one or two days.
- Resume at a lower dose once your INR comes down.
- Take 1 to 2.5 mg of oral vitamin K.
- Recheck INR in 24 hours.
- Get IV vitamin K (5-10 mg).
- Receive 4-factor prothrombin complex concentrate (PCC) to reverse the effect fast.
- Stop the antibiotic immediately.

Is There a Better Way?
Many people wonder: why not just switch to a newer blood thinner like apixaban or rivaroxaban? Those drugs-called DOACs-don’t interact with TMP-SMX the same way. They’re easier to manage, don’t need regular blood tests, and have fewer food interactions. But here’s the catch: not everyone can switch. People with mechanical heart valves still need warfarin. There’s no DOAC approved for them yet. And even among those who can switch, many don’t-because of cost, insurance coverage, or doctor preference. In 2022, 2.6 million Americans were still on warfarin. And TMP-SMX was the 47th most prescribed antibiotic in the U.S. That means this interaction isn’t going away anytime soon.What Patients Should Remember
If you’re on warfarin:- Always tell every doctor, pharmacist, and nurse you’re taking it-every time.
- Keep a list of all your meds, including over-the-counter drugs and supplements.
- Never start a new antibiotic without checking with your anticoagulation clinic or doctor.
- Know your target INR range and what your last result was.
- Don’t ignore small signs of bleeding. They’re early warnings.






Comments
Juliet Morgan
December 6, 2025 AT 11:29This is the kind of post that makes me want to hug the internet. Seriously, if you're on warfarin, please share this with your grandma, your uncle, your weird cousin who thinks antibiotics are candy. I've seen too many people get scared and stop their meds or worse, ignore the signs until it's too late. You just saved someone's life today. ❤️
Norene Fulwiler
December 6, 2025 AT 11:58I'm a nurse in rural Texas and I see this every single month. A patient comes in with a UTI, gets Bactrim, and two days later they're in the ER with a bleeding ulcer. No one tells them. No one warns them. We have to be the ones to say it. I wish every pharmacist would print a warning sticker on the bottle. Not just for warfarin - for all anticoagulants. This isn't just medical knowledge, it's a public health crisis waiting to happen.
Stephanie Bodde
December 7, 2025 AT 10:04Thank you for writing this. My mom had a near-miss last year. She took Bactrim for a sinus infection, didn't know about the interaction, and woke up with purple bruises all over her legs. We rushed her in - INR was 8.7. She’s fine now, but I’ll never forget the look on the ER doctor’s face when he saw her chart. I printed this out and taped it to the fridge. Everyone in my family knows now. 🙏
Annie Grajewski
December 8, 2025 AT 13:19Wow so let me get this straight - the same drug that kills your gut bacteria to treat a UTI also makes your blood turn into maple syrup? Genius. I bet Big Pharma loves this. They get paid for the antibiotic, the blood tests, the ER visits, the vitamin K, the PCC, the hospital stay… and you just sit there wondering why your co-pay is $400. #CapitalismHealthcare
ashlie perry
December 8, 2025 AT 20:18Did you know the FDA knew about this interaction since 1987? But they didn’t force warning labels because the drug companies said it was "too expensive to repackage." And now you’re telling us to be our own advocates? Yeah right. They want you scared, confused, and buying more meds. This isn’t medicine - it’s a control system. They don’t want you healthy. They want you dependent.
Mark Ziegenbein
December 9, 2025 AT 03:05Let me break this down for the laypeople who think "antibiotic" means "magic bullet" - this isn't just a pharmacokinetic interaction, it's a triple threat: protein binding displacement, CYP2C9 inhibition, and gut flora depletion. The S-warfarin enantiomer is particularly vulnerable due to its stereoselective metabolism, and when you combine that with trimethoprim's competitive inhibition of renal tubular secretion of creatinine - which indirectly alters volume of distribution - you get a pharmacodynamic cascade that's not just predictable, it's mathematically inevitable. And yet, we still let residents prescribe this like it's a birthday present. This is why evidence-based medicine needs to be mandatory in med school. No more "I think" - only "I measured".
Philip Kristy Wijaya
December 9, 2025 AT 12:18As a retired cardiologist with over forty years of clinical experience I must say that the author has presented an impeccably accurate and thoroughly researched analysis of this interaction. The data cited from the FDA and peer-reviewed studies is not only correct but essential. That said, I find it deeply troubling that such fundamental knowledge is not yet embedded into every primary care algorithm. The failure to implement standardized alerts in EHR systems is a dereliction of duty. We must demand better. The patient is not a statistic. The patient is a human being who deserves precision.
William Chin
December 11, 2025 AT 09:19My father died from a GI bleed in 2018 after being prescribed Bactrim for a UTI. He was 78. His INR was 11.2. The doctor said "it was just a coincidence." I spent three years fighting the hospital for answers. This post is the first thing that makes sense. Thank you. I wish I’d read this before it was too late.
Ada Maklagina
December 13, 2025 AT 05:27My INR spiked to 5.8 last winter after taking Bactrim. I didn’t know anything about this. I just thought I was getting sicker. Ended up in the ER. They gave me vitamin K. I felt fine the next day. But I didn’t tell anyone. Until now. I’m telling my mom. And my brother. And my yoga teacher. Everyone. This is too important to keep quiet.
Harry Nguyen
December 14, 2025 AT 19:20So you're telling me that a drug made in a lab by some foreign corporation can kill an American veteran on warfarin because we don't have enough "awareness"? That's not a medical problem - that's a national security failure. We let China and India make our meds and then wonder why our grandparents are bleeding out in ERs. We need to ban this antibiotic. Period. And bring back penicillin manufacturing. America First. Health First.
Rupa DasGupta
December 15, 2025 AT 15:15OMG I just gave my mom Bactrim last week and she’s on warfarin 😭 I didn’t know!! I’m so scared!! Should I rush her to the hospital?? I’m crying right now. Please help!! 🙏
Katie Allan
December 16, 2025 AT 21:34One of the most beautifully clear, compassionate, and clinically precise summaries of this interaction I’ve ever read. This isn’t just a post - it’s a public service. I’ve shared it with every patient I counsel on anticoagulation. I wish every pharmacy had a copy on their counter. Knowledge isn’t power - it’s protection. Thank you for giving people the tools to stay alive.
Laura Saye
December 17, 2025 AT 02:18There’s a deeper layer here that no one talks about - the existential vulnerability of being on warfarin. You’re not just managing a number. You’re living in a liminal space between life and death, where a single pill, a missed test, a well-meaning doctor’s oversight, can tip the scales. This interaction isn’t just chemical - it’s philosophical. It forces us to confront how fragile our bodies are, how dependent we are on systems that are often broken, and how deeply we must trust strangers with our survival. And yet, we do. We take the pill. We show up for the test. We hope. That’s not just medicine. That’s courage.