Diphenhydramine Overdose: Recognizing Antihistamine Toxicity and What to Do in an Emergency

Diphenhydramine Overdose Risk Calculator
Enter your weight and dose to determine overdose risk.
Based on medical guidelines: 5 mg/kg = danger threshold; 20 mg/kg = severe toxicity
What Happens When You Take Too Much Diphenhydramine?
Diphenhydramine is in almost every medicine cabinet. You’ve probably used it to help you sleep, calm an itchy rash, or fight allergies. Brands like Benadryl, Tylenol PM, and Sominex make it easy to get. But taking just a few extra pills can turn a harmless remedy into a life-threatening emergency. It’s not just about feeling sleepy-it’s about your heart, your brain, and your body shutting down.
Most adults take 25 to 50 mg every 4 to 6 hours. That’s safe. But when someone takes more than 5 mg per kilogram of body weight-say, 350 mg for a 70 kg adult-things start to go wrong. At 20 mg/kg or higher, you’re in danger of seizures, heart failure, or even death. And here’s the scary part: many people don’t realize how dangerous it is. They think, "It’s just an over-the-counter pill." That’s exactly why overdoses are rising.
The Anticholinergic Toxidrome: What Your Body Does When It’s Overloaded
When diphenhydramine floods your system, it blocks acetylcholine, a chemical your brain and body need to function. This causes a cluster of symptoms doctors call the anticholinergic toxidrome. There’s a simple way to remember it: Dry as a bone, red as a beet, blind as a bat, mad as a hatter, hot as hades, full as a flask.
- Dry as a bone: Your mouth feels like sandpaper. You can’t swallow. Your eyes are parched.
- Red as a beet: Your skin turns flushed and warm-sometimes hot enough to burn.
- Blind as a bat: Your pupils dilate, don’t react to light, and you can’t focus. Everything looks blurry or double.
- Mad as a hatter: You’re confused, agitated, or hallucinating. You might see people who aren’t there. You might think you’re in a different room, or even a different time.
- Hot as hades: Your body temperature spikes. Over 104°F (40°C) isn’t rare. This isn’t just a fever-it’s a medical crisis.
- Full as a flask: You can’t pee. Your bladder swells. Catheters become necessary.
These aren’t side effects. They’re signs your central nervous system is being overwhelmed. And if you’re not treated fast, it gets worse.
When It Turns Life-Threatening: Seizures, Heart Problems, and Organ Failure
At doses above 20 mg/kg, diphenhydramine starts acting like a tricyclic antidepressant overdose. It blocks sodium channels in your heart. That’s the same mechanism that can kill someone after taking too many antidepressants.
On an EKG, you’ll see two red flags:
- QRS widening over 100 ms: This means your heart’s electrical signal is slowing down. It’s a sign of severe toxicity. Without treatment, this can lead to ventricular arrhythmias or cardiac arrest.
- QTc prolongation over 500 ms: This increases your risk of torsades de pointes-a dangerous, potentially fatal heart rhythm.
Seizures happen in 15 to 20% of severe cases. Delirium can turn into full-blown psychosis. Some patients develop rhabdomyolysis-muscle tissue breaks down, floods the bloodstream with toxins, and can shut down your kidneys. One case in the literature showed a creatine phosphokinase level of 18,000 U/L. That’s 30 times the normal limit.
And yes, people have died from this. The mortality rate is low-around 0.5%-but it’s real. Most deaths happen when people delay care or don’t recognize the signs.

What Emergency Teams Do When You Arrive at the Hospital
If someone overdoses on diphenhydramine, the ER doesn’t wait. They start with ABCDE: Airway, Breathing, Circulation, Disability, Exposure. They check your vitals. They hook you to a cardiac monitor. They draw blood-not for diphenhydramine levels (those don’t help), but to check for acetaminophen (since Tylenol PM combines both), kidney function, and muscle damage.
Here’s what actually saves lives:
- Benzodiazepines (diazepam or lorazepam): First-line for seizures and agitation. They calm the brain without worsening heart problems.
- Sodium bicarbonate: Given IV if the QRS complex is wider than 100 ms. It pushes sodium back into heart cells and stabilizes rhythm.
- Magnesium sulfate: Used if QTc is over 500 ms to prevent torsades.
- Physostigmine: This is the game-changer. It reverses the anticholinergic effects in the brain. A 2021 study showed 87% of patients with severe delirium improved with physostigmine, compared to just 24% with benzodiazepines alone. It’s not used if the patient has seizures or heart block-but when it’s safe, it works fast.
- Active cooling: Ice packs, fans, cool IV fluids-anything to bring down that dangerous fever.
- Urinary catheter: If you can’t pee, they put one in. Simple, but essential.
Some extreme cases need lipid emulsion therapy or even ECMO-a machine that takes over heart and lung function. These are last-resort measures, but they’ve brought people back from the edge.
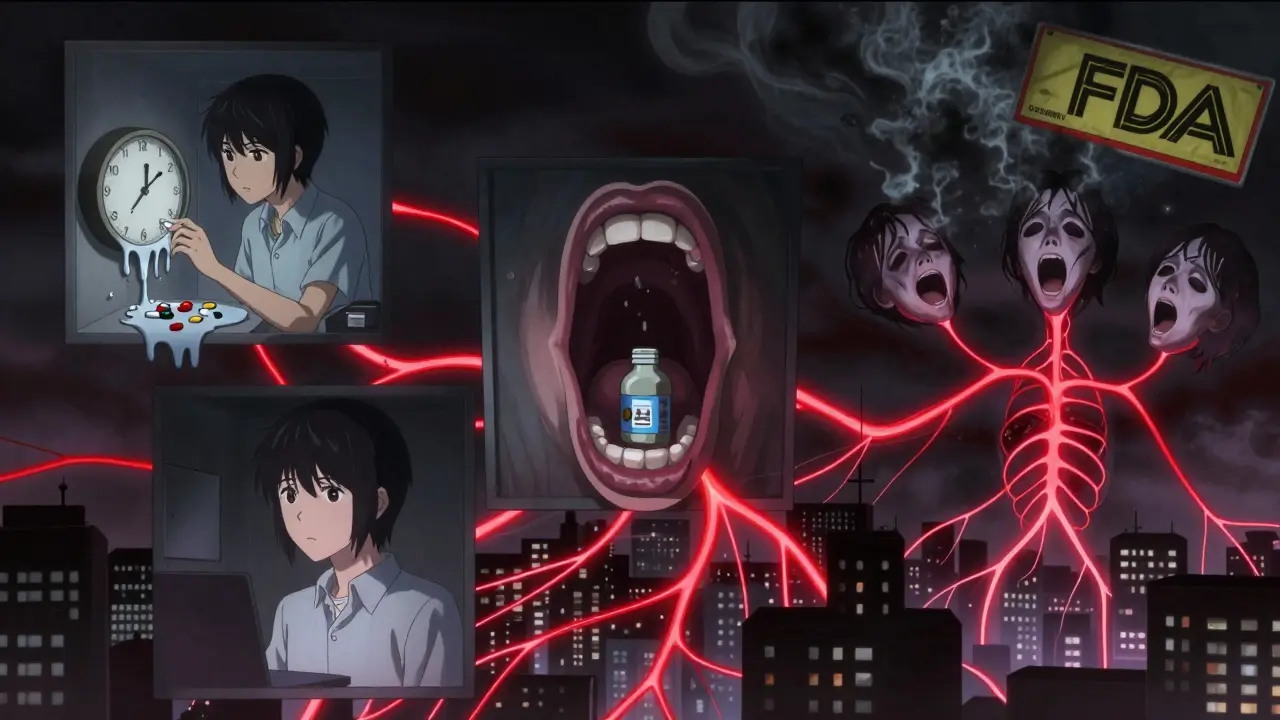
Why So Many Teens Are Dying From Benadryl Challenges
Between 2018 and 2022, intentional diphenhydramine overdoses in teens tripled. Why? Social media. TikTok, Reddit, and YouTube are full of videos titled "Benadryl Challenge"-where people take 300, 500, even 600 mg to get high. Users describe "terrifying hallucinations," "being unable to move," and "waking up in the ER with a catheter." One Reddit user wrote: "I thought I could get high. I didn’t know I’d almost die."
The FDA and American Academy of Pediatrics have launched campaigns like "Don’t Take the Benadryl Challenge," but the videos keep coming. Poison control centers report that 68% of overdoses happen in people under 20. A quarter of those are young children who accidentally swallowed pills. Nearly half are teens trying to escape reality.
It’s not just dangerous-it’s addictive. Some users report returning to it because the hallucinations feel "real" or "spiritual." That’s not a trip. That’s brain poisoning.
What to Do If You Suspect an Overdose
If you think someone has taken too much diphenhydramine:
- Call 911 immediately. Don’t wait for symptoms to get worse.
- Call Poison Control at 1-800-222-1222. They’ll guide you while you wait for EMS.
- Don’t induce vomiting. It’s not helpful and can cause choking.
- Keep the person awake and cool. If they’re hot, remove clothes, use fans. If they’re seizing, protect their head, turn them on their side.
- Bring the pill bottle. Even if it’s empty. The packaging tells doctors what else was in the pill.
Don’t assume it’s "just a bad trip." It’s not. It’s a medical emergency that needs IV meds, cardiac monitoring, and often ICU-level care.
Recovery and Long-Term Risks
Most people recover fully if treated early. But recovery isn’t instant. Sedation can last 24 to 48 hours. Confusion lingers for days. Some people have memory gaps. Others report lasting anxiety or difficulty concentrating.
Those who had seizures or cardiac issues need follow-up with a cardiologist. Rhabdomyolysis can cause permanent kidney damage. And if this was intentional, mental health support is critical. Many teens who overdose on diphenhydramine are struggling with depression, anxiety, or trauma.
The good news? With timely care, survival rates are high. Emergency teams in Chicago, Boston, and Portland report near-total recovery in cases where treatment started within 4 hours. The key is acting before the heart or brain takes irreversible damage.
How to Prevent This From Happening
- Store all medications out of reach-even "harmless" ones. Children don’t know the difference between candy and medicine.
- Never use diphenhydramine as a sleep aid long-term. It loses effectiveness and increases fall risk in older adults.
- Read labels. Tylenol PM, ZzzQuil, Unisom, and many cold medicines contain diphenhydramine. Taking more than one can easily lead to overdose.
- Talk to teens. Don’t assume they know the risks. Show them real cases. Show them EKGs. Show them what a catheter looks like after a Benadryl overdose.
- Download the Poison Help app. It’s free, works offline, and connects you to poison control in seconds.
Diphenhydramine isn’t the villain. It’s a tool. But like any tool, misuse turns it into a weapon. The best defense? Knowledge. And action-before it’s too late.






Comments
Josh Potter
December 17, 2025 AT 10:14Bro i took 6 Benadryl last week just to see what happened. Thought i was gonna fly. Ended up in the ER with a catheter and my mom crying. Don't be dumb. This shit ain't a vibe.
Evelyn Vélez Mejía
December 17, 2025 AT 17:17The anticholinergic toxidrome is not merely a collection of symptoms-it is the silent unraveling of the autonomic nervous system, a biochemical betrayal orchestrated by a substance so ubiquitously trivialized as to be nearly sacred in American households. To dismiss diphenhydramine as 'just an antihistamine' is to confuse a scalpel with a butter knife-and then wonder why the patient bled out.
Victoria Rogers
December 18, 2025 AT 21:31This article is so woke. Like, why are we even talking about this? People die from too much sugar too. Should we ban soda? Benadryl is fine. It's the parents who don't lock up medicine. Also, TikTok is fake. I know a guy who did 800mg and he's fine. Chill out.
Jane Wei
December 20, 2025 AT 07:27I used to take 100mg every night to sleep. Didn't think twice. Then one night I couldn't move my eyes and thought my dog was talking to me. That was the last time. Scary as hell.
Erik J
December 22, 2025 AT 02:23Is there any data on the correlation between long-term diphenhydramine use and cognitive decline in older adults? I recall a 2019 JAMA study suggesting an association, but it wasn't mentioned here.
BETH VON KAUFFMANN
December 23, 2025 AT 22:00The QRS widening criterion is oversimplified. The true diagnostic threshold is 120ms in the context of sodium channel blockade, not 100ms. Also, physostigmine is not 'game-changing'-it's high-risk and contraindicated in >40% of cases. This article reads like a marketing pamphlet for poison control.
Michael Whitaker
December 25, 2025 AT 19:13I'm a physician in Boston. I've seen this 17 times in the last year. The real issue? Parents don't know what's in their own medicine cabinet. And teens? They think hallucinating for 12 hours is 'spiritual.' It's not. It's neurotoxicity. And no, you can't 'tough it out.'
Marie Mee
December 27, 2025 AT 17:12This is all a hoax. The government wants us to think OTC meds are dangerous so we'll buy their expensive prescriptions. Benadryl is natural. The real poison is Big Pharma. They put fluoride in the water too. I know a guy who took 200 pills and woke up on a beach in Mexico. Coincidence?
Naomi Lopez
December 28, 2025 AT 12:33The phrasing 'mad as a hatter' is culturally reductive and historically inaccurate. The phrase originates from mercury poisoning in 19th-century hatmakers-not anticholinergic toxicity. Please consult a medical historian before using metaphorical tropes in clinical communication.
Salome Perez
December 28, 2025 AT 19:46In my work in rural clinics across the Southwest, I've seen this happen more than you'd think. Grandmas mixing Tylenol PM with their blood pressure meds. Teens thinking it’s a party trick. The tragedy isn’t the drug-it’s the silence around it. We need to talk about this in schools, churches, barbershops. Not just ERs.
Kent Peterson
December 30, 2025 AT 08:29This is why America is collapsing. We let kids do whatever they want. In my day, if you took too much Benadryl, you got a belt and a lecture. Now? We write 2,000-word articles about it. And the FDA? They’re too busy banning bubble tea. This isn't a crisis-it's a character flaw.
Meghan O'Shaughnessy
December 31, 2025 AT 16:45I work in a pharmacy. We hand out Benadryl like candy. People ask for it for their dogs, their kids, their hangovers. No one ever reads the label. We should have warning stickers. Like on cigarette packs.
Kaylee Esdale
January 1, 2026 AT 03:57My little brother did this. He’s 16. He thought it was like weed. He didn’t know he was almost dead. We’re in therapy now. If you’re reading this and you’re thinking about trying it-don’t. You won’t feel free. You’ll feel trapped in your own head. And you’ll never forget it.