How Age Affects Medication Side Effects and Tolerability in Older Adults
Medication Safety Calculator for Older Adults
How Age Affects Your Medication Safety
This tool estimates your risk of medication side effects based on age and common drug types. It's not medical advice but helps identify potential concerns.
Recommendations
- ✓ Continue current regimen
- ℹ️ Schedule medication review in 6 months
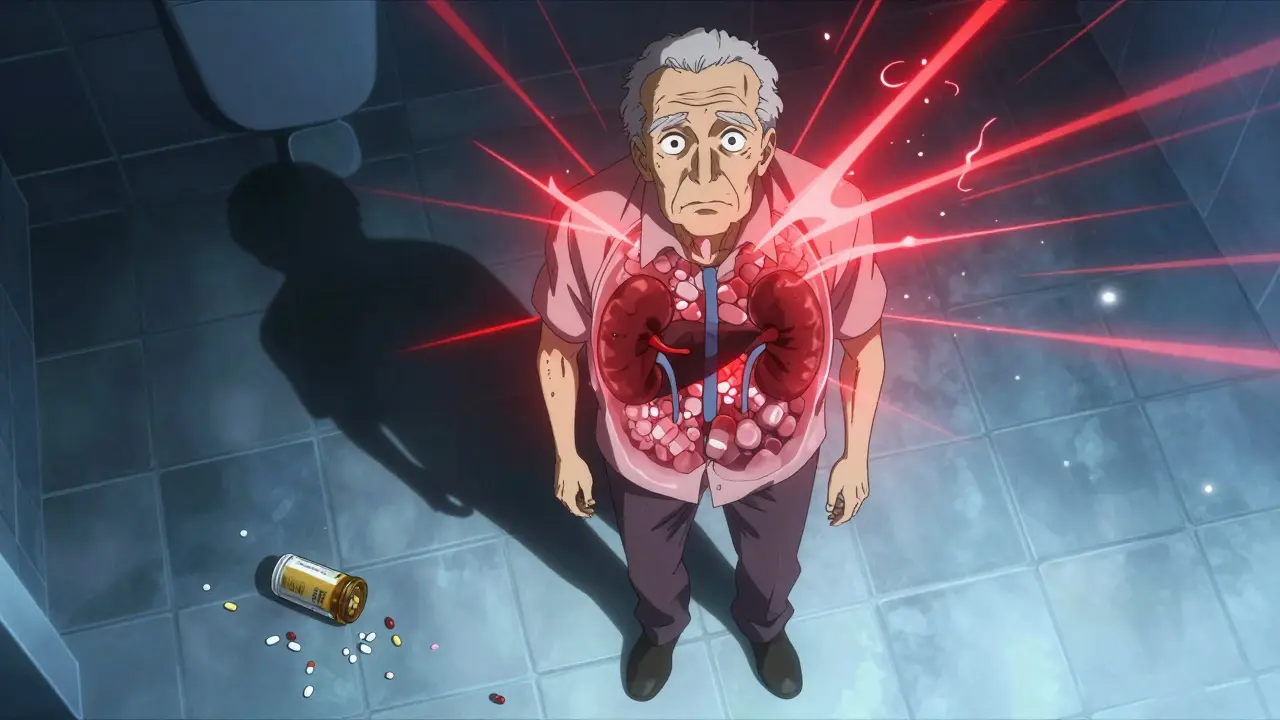
When you’re 70, a pill that once helped you sleep might leave you confused, dizzy, and on the floor. That’s not just bad luck-it’s biology. As we age, our bodies change in ways that make medications behave differently, often turning helpful treatments into dangerous ones. The same dose that worked at 40 can become toxic at 75. This isn’t speculation. It’s backed by decades of research, clinical data, and real patient stories.
Why Older Bodies Handle Drugs Differently
Your body doesn’t just slow down with age-it reorganizes. Between ages 25 and 80, total body water drops by about 15%, while body fat climbs from 25% to nearly 50% in women. This changes how drugs move through your system. Water-soluble drugs like lithium or digoxin become more concentrated because there’s less fluid to dilute them. Fat-soluble drugs like diazepam or fluoxetine linger longer because they get stored in fatty tissue and released slowly over time. Your kidneys, the main filters for most medications, also decline. After age 40, your glomerular filtration rate (GFR) drops by about 0.8 mL/min per year. By 70, you might be processing drugs at half the speed of a 30-year-old. That means drugs like warfarin, aminoglycosides, or metformin stick around longer, increasing the risk of overdose-even if you take the same dose. Your liver isn’t working as hard either. Blood flow to the liver drops by 20-40% between 25 and 65. That affects drugs like propranolol and verapamil, which rely on liver enzymes to break them down. The result? Higher blood levels, longer duration, and more side effects. Then there’s protein binding. Albumin, the main protein that carries drugs like warfarin and phenytoin through the blood, decreases by 10-15% in older adults. That means more of the drug is floating around unbound-and active. Even a normal dose can become too strong.Brain and Body Get More Sensitive
It’s not just how your body handles drugs-it’s how your brain and organs respond to them. Older adults are far more sensitive to the effects of medications on the central nervous system. A 2023 study showed that older people get 50% more sedation and memory problems from diazepam than younger adults, even when blood levels are identical. Beta-blockers like propranolol need 50% higher doses in younger people to achieve the same heart rate reduction. But in older adults, even low doses can cause dangerously slow heart rates or dizziness. The same goes for opioids. Fentanyl and alfentanil require 30-50% lower doses in older patients to avoid respiratory depression. Anticholinergic drugs-commonly found in allergy meds, sleep aids, and even some antidepressants-can trigger sudden confusion, delirium, or memory loss in older adults. A University of Florida study found that people over 75 are 4.2 times more likely to experience delirium from these drugs than those under 65. That’s why medications like diphenhydramine (Benadryl) and oxybutynin are on the Beers Criteria list of drugs to avoid in older adults.Common Medications That Become Risky with Age
Some drugs are fine for younger people but become dangerous after 65. Here are a few that show up again and again in hospital admissions:- Benzodiazepines (like lorazepam, alprazolam): 2-3 times higher risk of falls and hip fractures. Zolpidem causes 80% more next-day drowsiness in people over 65.
- NSAIDs (like ibuprofen, naproxen): Increase risk of stomach bleeding and kidney failure. One study found 28% of older adults on NSAIDs developed acute kidney injury within 30 days.
- Anticholinergics (diphenhydramine, oxybutynin, amitriptyline): Linked to cognitive decline, urinary retention, and constipation. Amitriptyline alone caused urinary retention severe enough to require catheterization in 1 in 10 older men.
- Proton pump inhibitors (omeprazole, pantoprazole): Long-term use increases risk of bone fractures, infections like C. diff, and low magnesium levels.
- Antihypertensives (especially diuretics and ACE inhibitors): Cause orthostatic hypotension in 28% of people over 80-compared to just 9% in those 50-65.
The Beers Criteria is a widely used list of potentially inappropriate medications for older adults, updated every two years by the American Geriatrics Society. The 2023 version identifies 56 drugs and drug classes that carry higher risks than benefits for people over 65. It’s not a ban-it’s a warning. Many of these drugs are still prescribed because doctors aren’t aware, or because the patient’s history makes them seem necessary.
Polypharmacy: The Hidden Danger
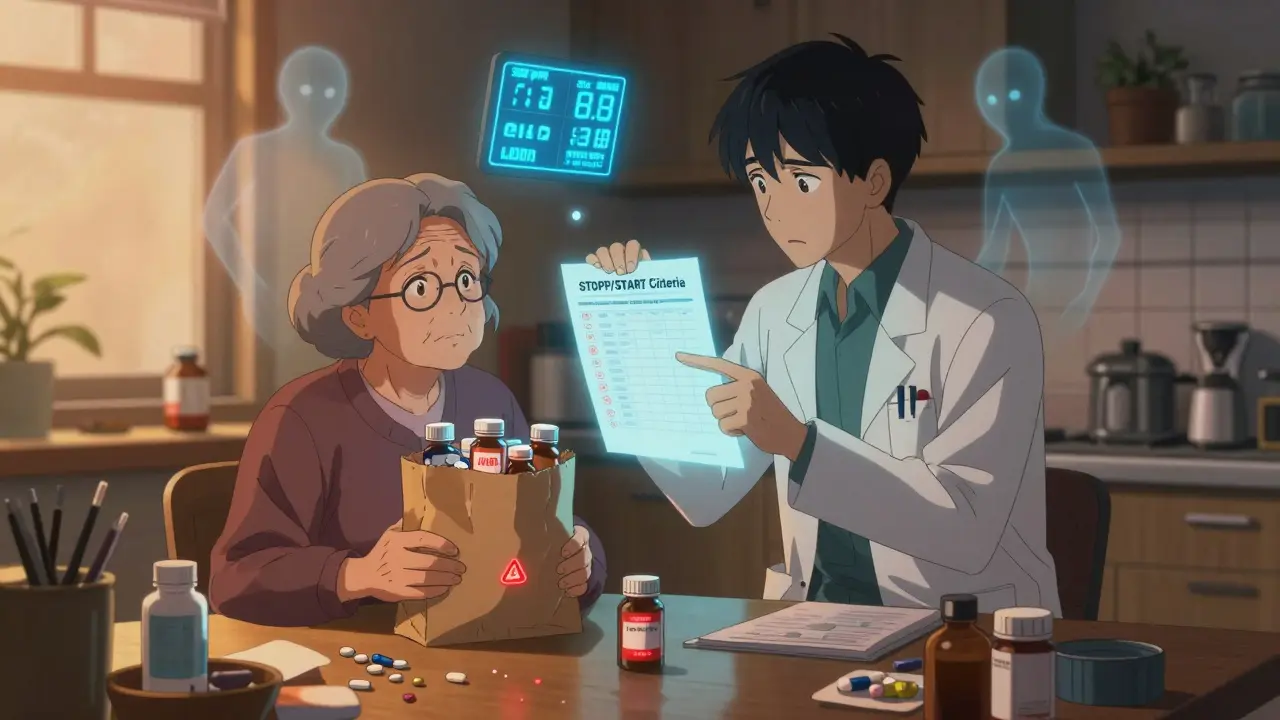
Nearly half of adults over 65 take five or more prescription drugs every month. That’s called polypharmacy. It’s not just about the number of pills-it’s about how they interact. One drug might slow the metabolism of another. Another might raise blood pressure, forcing a second drug to counter it. The more pills you take, the higher the chance of a bad reaction. A 2022 study found that patients taking 10 or more medications had a 75% chance of experiencing at least one adverse drug reaction in a year. And it’s not always obvious. Dizziness might be blamed on old age. Confusion might be labeled as early dementia. But often, it’s just a drug interaction. That’s why STOPP/START criteria are so important. Developed by Dr. Joseph T. Hanlon and colleagues, these guidelines help doctors identify which medications to stop (STOPP) and which ones to start (START) in older adults. For example, STOPP says: stop long-term benzodiazepines in someone with a history of falls. START says: add a statin if they have heart disease and no contraindications.Real Stories Behind the Data
Behind every statistic is a person. On Reddit, a 78-year-old man described how amitriptyline-prescribed for nerve pain-led to urinary retention so severe he needed a catheter within days. On AgingCare.com, a daughter wrote that her 82-year-old mother fractured her hip after being prescribed the same blood pressure dose used for a 50-year-old. A 2022 survey of 1,200 older adults found that 68% had experienced dizziness or falls linked to meds. 54% reported memory problems. 41% had unexplained weight loss or gain. And 45% admitted they’d stopped taking a medication because the side effects were worse than the condition it was treating. These aren’t rare cases. They’re the norm.
What Can Be Done?
The good news? Many of these problems are preventable.- Start low, go slow. Initial doses for older adults should be 25-50% of standard adult doses, especially for drugs cleared by the kidneys.
- Review meds every 3-6 months. The American Medical Association recommends full medication reviews for anyone over 65 on multiple drugs. Bring all pills-prescription, OTC, supplements-to your appointment. Pharmacists call this a "Brown Bag Review." They find an average of 3.2 discrepancies per patient.
- Use eGFR, not just creatinine. Kidney function can’t be judged by blood tests alone. Always use the CKD-EPI equation to calculate your true filtration rate.
- Deprescribe when possible. If a drug was started for a condition that’s no longer relevant-like a blood thinner for a past atrial fibrillation episode-it’s time to stop.
- Ask about alternatives. Is there a non-drug option? For sleep, try sleep hygiene before zolpidem. For pain, try physical therapy before NSAIDs.
Some hospitals now use AI tools like MedAware to flag dangerous combinations before prescriptions are filled. The FDA has approved 37 new age-adjusted medications since 2020. And by 2026, Medicare may require universal medication reviews for all beneficiaries.
What You Can Do Today
You don’t need to wait for a doctor’s appointment to protect yourself.- Keep a written list of every medication you take, including doses and why you take them.
- Ask your pharmacist: "Is this still right for me?"
- If you feel dizzy, confused, or unusually tired after starting a new drug, don’t wait-call your doctor.
- Don’t be afraid to say: "I think this medication is making me worse." Many side effects are reversible if caught early.
Medications aren’t harmless. Especially as we age, they become more like fine-tuned tools than blunt instruments. The right dose can save a life. The wrong one can end it. The goal isn’t to avoid all drugs-it’s to use them wisely, with awareness, and with a plan.
Why do older adults have more side effects from the same medication dose?
As we age, our bodies change: kidneys filter slower, liver metabolism drops, body fat increases, and brain sensitivity rises. These changes mean drugs stay longer in the body and have stronger effects-even at the same dose. A pill that was safe at 50 can become dangerous at 75.
What is the Beers Criteria and why does it matter?
The Beers Criteria is a list of medications that pose higher risks than benefits for adults over 65. Updated every two years by the American Geriatrics Society, it helps doctors avoid drugs like diphenhydramine, benzodiazepines, and NSAIDs that commonly cause falls, confusion, or kidney damage in older adults. It’s not a rulebook-it’s a safety guide.
How many medications are too many for older adults?
There’s no magic number, but taking five or more medications increases the risk of side effects by 50%. Taking 10 or more raises the chance of a serious adverse reaction to 75% in a year. The goal isn’t to take fewer pills-it’s to take only the ones that still benefit you.
Can I stop my medication if I think it’s causing side effects?
Never stop a medication suddenly without talking to your doctor. Some drugs, like blood pressure or antidepressant meds, can cause dangerous withdrawal effects. But if you’re feeling worse, tell your doctor immediately. Many side effects are reversible, and there are often safer alternatives.
Are over-the-counter drugs safe for older adults?
Not always. Many OTC meds contain anticholinergics (like diphenhydramine in sleep aids) or NSAIDs (like ibuprofen), which are high-risk for older adults. Even "natural" supplements can interact with prescriptions. Always check with your pharmacist before taking anything new.
What’s the best way to prevent medication problems as I age?
Keep a current list of all medications, review them with your doctor or pharmacist every 3-6 months, ask if each drug is still needed, and report any new symptoms like dizziness, confusion, or falls. Use the Brown Bag Review method and ask about deprescribing options. Prevention is always better than treatment.






Comments
Erika Putri Aldana
December 21, 2025 AT 07:29This is just Big Pharma pushing pills to keep old people hooked. They don't care if you fall or get confused-they just want your insurance to keep paying. I've seen it firsthand: my grandma was on 12 meds, and half were just for side effects of the other half. They profit from your decline.
Adrian Thompson
December 22, 2025 AT 05:03Oh great, another ‘geriatric guidelines’ pamphlet. Let me guess-next they’ll tell us to stop breathing because our lungs are ‘too old.’ The real problem? Doctors haven’t been trained to think for themselves since the 90s. If your kidney function’s down, adjust the dose-not ban the drug. One-size-fits-all medicine is why we’re all dying slower and more expensively.
Cameron Hoover
December 22, 2025 AT 08:39I just want to say-this post saved my dad’s life. He was on benzos and NSAIDs for years. Dizzy all the time. Thought it was just ‘getting old.’ We did the Brown Bag Review with his pharmacist and cut 4 meds. He’s walking without a cane now. It’s not magic. It’s just paying attention. Thank you for writing this. Seriously.
Teya Derksen Friesen
December 24, 2025 AT 04:21While the empirical data presented herein is both compelling and methodologically robust, it remains insufficiently contextualized within the broader socio-economic determinants of pharmaceutical overprescription in aging populations. The systemic failure lies not in pharmacokinetic variables alone, but in the commodification of geriatric care under neoliberal healthcare paradigms. Deprescribing, while clinically prudent, is rendered structurally infeasible without institutional reform.
Sandy Crux
December 24, 2025 AT 17:54...and yet, nobody mentions that 87% of these "dangerous" drugs were prescribed by specialists who never even reviewed the patient’s full med list... Also, the Beers Criteria? That’s just a list of drugs that Big Pharma doesn’t own the patent to anymore. Interesting how the "safety guidelines" always align with generic drug promotion, isn’t it? ...just saying.
Hannah Taylor
December 24, 2025 AT 20:41my mom took benadryl for sleep and started talkin to her dead cat. i thought she was goin crazy. turns out it was the med. i told her to stop and she said "but the dr said it was safe!". yeah right. drs are just guessin half the time anyway. now she takes melatonin and sleeps like a baby. also, no more ibuprofen. kidneys arent invincible.
Jay lawch
December 25, 2025 AT 00:54Let’s be honest: this isn’t about biology. It’s about control. The medical-industrial complex has spent decades convincing older people they’re broken, so they’ll keep buying pills. In India, we’ve seen this before-colonial medicine told us our bodies were inferior, and now Western medicine tells our elders they’re too fragile for their own good. The truth? Older bodies aren’t failing-they’re being poisoned by profit-driven protocols. We don’t need more guidelines. We need less prescribing. Less corporate influence. More respect. And no, I won’t be taking your pills.
Jason Silva
December 25, 2025 AT 12:05My uncle was on 11 meds. Now he’s on 3. He plays guitar again. 🎸 Life’s too short for side effects. Talk to your pharmacist. Ask questions. Don’t be shy. Your body isn’t a vending machine. And if you feel weird after a new script? Stop. Call. Survive. 💪❤️