Insulin and Beta-Blockers: What You Need to Know About Hypoglycemia Unawareness

Hypoglycemia Risk Assessment Tool
Assess Your Risk
Enter your information to see your personalized hypoglycemia risk assessment.
When you’re managing diabetes with insulin, your body already walks a tightrope between too much and too little blood sugar. Now add a beta-blocker - a common heart medication - and that tightrope gets even narrower. Many people don’t realize that these two drugs, often prescribed together, can silently increase the risk of life-threatening low blood sugar episodes. The danger isn’t just that blood sugar drops - it’s that you might not feel it coming.
Why Hypoglycemia Unawareness Is So Dangerous
Hypoglycemia unawareness means your body stops giving you the usual warning signs of low blood sugar. Normally, when your glucose drops, your body releases adrenaline. That’s what causes shaking, a racing heart, sweating, and anxiety - signals that tell you to eat something fast. But in people with long-term diabetes, especially type 1, repeated low blood sugar episodes can dull these responses over time. Add beta-blockers into the mix, and those signals vanish entirely.Studies show that about 40% of people with type 1 diabetes develop hypoglycemia unawareness. For those on insulin, this isn’t just inconvenient - it’s deadly. Without warning, blood sugar can plummet to dangerous levels, leading to confusion, seizures, coma, or even death. And because beta-blockers block adrenaline, the most reliable early signs - like a pounding heartbeat or trembling hands - disappear. You’re left with no alarm clock to wake you up before it’s too late.
How Beta-Blockers Mask the Signs
Not all beta-blockers are the same. There are two main types: selective (cardioselective) and non-selective. Selective ones, like metoprolol and atenolol, mainly target the heart. Non-selective ones, like propranolol, affect the whole body, including the liver and muscles.Here’s the key point: beta-blockers don’t stop low blood sugar from happening. They stop you from feeling it. Adrenaline-driven symptoms - heart palpitations, shaking, and nervousness - are suppressed because beta-blockers block the receptors that adrenaline acts on. But here’s what most people don’t know: sweating is still possible. That’s because sweating is controlled by a different system - acetylcholine, not adrenaline. So if you’re on a beta-blocker and start sweating for no reason, especially if you’re on insulin, that’s your last warning sign. Don’t ignore it.
Research from 2019 shows that people taking selective beta-blockers have 2.3 times higher odds of experiencing hypoglycemia compared to those not on them. And while non-selective beta-blockers are worse at masking symptoms, even the "safer" selective ones carry real risk. One study found that 68% of hypoglycemic events in hospitalized diabetic patients on beta-blockers happened within the first 24 hours - often when glucose checks were infrequent or skipped.
The Hidden Metabolic Impact
It’s not just about masking symptoms. Beta-blockers also interfere with your body’s ability to fix low blood sugar on its own. Normally, when glucose drops, your liver releases stored sugar (glycogen) to bring levels back up. Beta-blockers, especially those that block beta-2 receptors, shut down that process. They also reduce insulin clearance, meaning insulin sticks around longer than it should. This double hit - no warning signs + no natural correction - makes hypoglycemia more severe and harder to recover from.That’s why some studies show that people on selective beta-blockers have a 28% higher risk of dying from hypoglycemia compared to those not taking them. The risk isn’t theoretical. In hospitals, where glucose levels are monitored closely, beta-blocker use still leads to frequent and dangerous lows. Outpatient settings are even more dangerous - people often check their blood sugar only once or twice a day. If you’re on insulin and a beta-blocker, that’s not enough.

Carvedilol: A Safer Choice?
Not all beta-blockers are created equal when it comes to diabetes. Carvedilol, a non-selective beta-blocker with additional alpha-blocking properties, stands out. Unlike metoprolol or atenolol, carvedilol doesn’t seem to raise the risk of hypoglycemia as much. In fact, one 2022 guideline found that carvedilol was linked to a 17% lower rate of severe hypoglycemia compared to metoprolol in diabetic patients.Why? Carvedilol has antioxidant effects and may preserve some of the body’s natural glucose recovery mechanisms. It also doesn’t suppress glucagon release as much as other beta-blockers. For someone with diabetes who needs a beta-blocker - say, after a heart attack - carvedilol is increasingly becoming the preferred option. The American College of Cardiology now recommends it as a first-line choice for diabetic patients with cardiovascular disease, especially if they’ve had hypoglycemia before.
What You Should Do Right Now
If you’re on insulin and a beta-blocker, here’s what you need to do immediately:- Check your blood sugar more often. At least four times a day - before meals and at bedtime. If you’re hospitalized, checks every 2-4 hours are standard.
- Use continuous glucose monitoring (CGM). CGM use has grown 300% since 2018 in this group, and it cuts severe hypoglycemia by 42%. If you don’t have one, talk to your doctor. It’s not a luxury - it’s a safety tool.
- Know your last warning sign: sweating. If you break out in sweat for no reason, check your glucose. Don’t wait for shaking or dizziness - those might not come.
- Avoid non-selective beta-blockers like propranolol. If you’re on one, ask if switching to carvedilol or a selective beta-blocker is an option.
- Teach your family and friends. If you lose consciousness from low blood sugar, they need to know to give you glucagon or call 999. Never assume someone will notice you’re unwell.
What About Long-Term Risk?
Some studies, like the ADVANCE trial, suggest that over five years, the risk of severe hypoglycemia may not be much higher in people on beta-blockers compared to placebo. But here’s the catch: those studies were done in stable outpatient settings with careful monitoring. They don’t reflect the real-world chaos - missed meals, illness, sudden activity changes, or sleep-time lows.The truth is, the biggest danger happens in the short term: the first few days after starting a beta-blocker, or after a change in insulin dose. That’s when the body hasn’t adjusted, and the masking effect hits hardest. One hospital study found that 72% of hypoglycemic events in diabetic patients on beta-blockers occurred during these transitional periods.
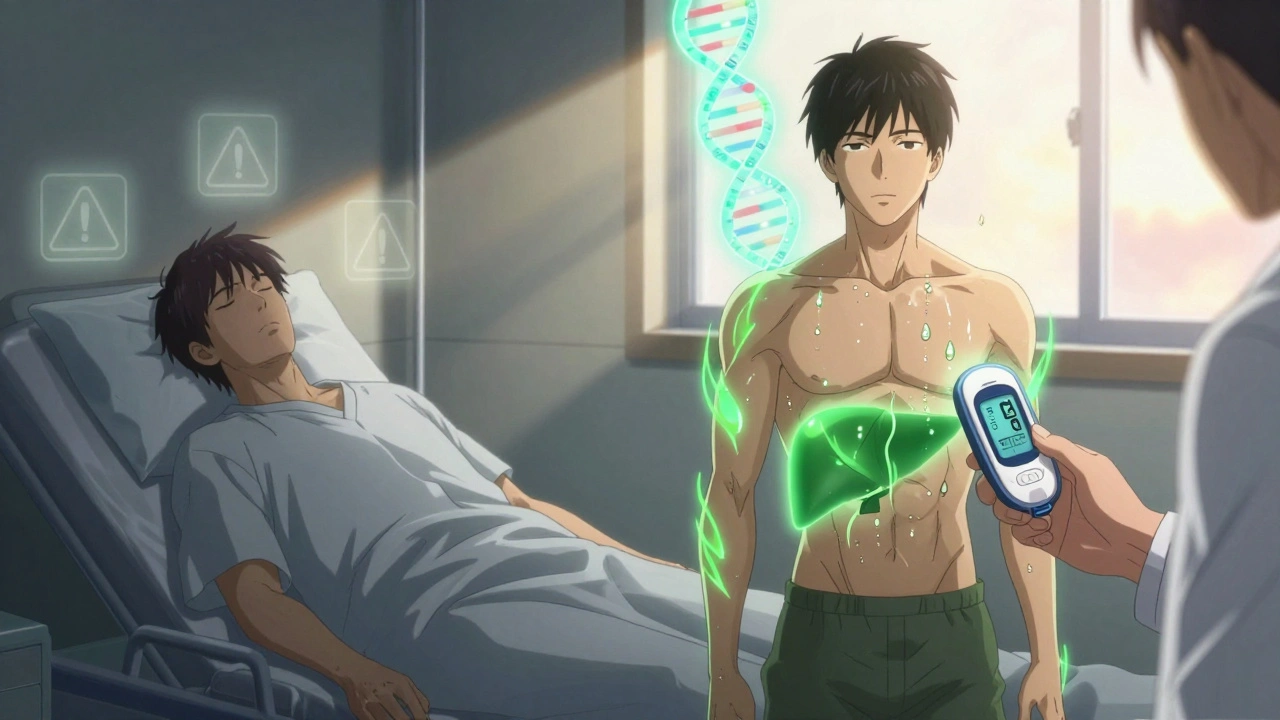
The Future: Personalized Medicine
Researchers are now looking at genetic markers that might predict who’s most likely to develop hypoglycemia unawareness on beta-blockers. The DIAMOND trial, launched in 2023, is testing whether certain gene variants make people more sensitive to the masking effects. If successful, this could mean future prescriptions aren’t one-size-fits-all. Instead, your DNA might help your doctor choose the safest beta-blocker for you.In the meantime, the best strategy is simple: don’t assume safety. Don’t rely on symptoms. Use technology. Choose the right drug. Monitor constantly. And never underestimate the quiet danger of a drug that steals your warning system.
What to Ask Your Doctor
- "Am I on the safest beta-blocker for my diabetes?"
- "Should I switch to carvedilol?"
- "Can I get a continuous glucose monitor?"
- "What should I do if I start sweating without a reason?"
- "Do I need to change my insulin dose now that I’m on this medication?"
These aren’t optional questions. They’re survival questions.






Comments
Sheryl Lynn
December 2, 2025 AT 03:25Oh sweet merciful heavens, this is the kind of post that makes me want to hug my CGM and whisper sweet nothings to it at 3 a.m. I was on metoprolol for six months and thought my ‘weird sweating episodes’ were just stress-induced menopause vibes. Turns out? My body was screaming into a void while my beta-blocker muted the alarm. I nearly passed out during a Zoom call. Never again. Carvedilol saved my life. Also, if you’re not using a CGM, you’re basically playing Russian roulette with your pancreas. 🤡
Paul Santos
December 3, 2025 AT 06:00Interesting. The epistemological rupture between autonomic signaling and pharmacological modulation is profound here. Beta-blockers don’t merely mask symptoms-they perform a kind of phenomenological erasure of interoceptive awareness. It’s almost Heideggerian: Dasein loses its ability to be-toward-blood-glucose. And yet, the sweat remains-a Lacanian leftover, a symptom of the Real breaking through the symbolic order. 🤔
Eddy Kimani
December 4, 2025 AT 10:03Just want to add some clinical context: the 2.3x increased odds of hypoglycemia with selective beta-blockers comes from a 2019 JAMA Internal Medicine meta-analysis of over 12,000 patients. But here’s the kicker-those numbers jump to 4.1x if the patient is also on SGLT2 inhibitors. We’re seeing a perfect storm in older T1Ds on combo therapy. Also, glucagon kits are still underutilized. If your family doesn’t know how to use one, you’re not just at risk-you’re a liability. Get trained. Now.
Chelsea Moore
December 5, 2025 AT 08:48HOW DARE YOU NOT CHECK YOUR BLOOD SUGAR FOUR TIMES A DAY?!?!?!?!?!!! I have a friend who went into a coma because she thought ‘it was just a headache’-and she was on PROPRANOLOL!!! This is not a suggestion. This is not a ‘maybe.’ This is a death sentence if you ignore it. I’m not mad-I’m just disappointed. And also, why are you still using fingersticks?!? CGM is not a luxury-it’s a lifeline. I’m crying. I’m literally crying.
John Biesecker
December 5, 2025 AT 08:58man this hits different. i used to think sweating meant i was hot or anxious… turns out it was my body screaming ‘HELP I’M DYING’ and i just brushed it off like ‘oh chill’ 🥲. now i’ve got a dexcom glued to my arm and i check it like it’s my ex’s texts-constantly, nervously, hoping it’s not dropping. carvedilol changed my life. also, if you’re on beta-blockers and don’t have a glucagon pen… go get one. your future self will thank you. 🙏
Allan maniero
December 6, 2025 AT 13:26There’s something quietly tragic about how modern medicine gives us so many tools to survive, yet we still rely on the body’s old warning systems-systems that drugs have quietly disabled. It’s not that we’re careless; it’s that we’re taught to trust symptoms. But when the body stops speaking, we’re left with silence-and silence is the most dangerous thing in a diabetic’s life. I’ve seen too many people lose consciousness thinking they’re fine. The answer isn’t more willpower. It’s more technology. More awareness. More humility.
Anthony Breakspear
December 6, 2025 AT 14:43Bro. I used to be the guy who skipped checks because ‘I felt fine.’ Then I blacked out in the grocery store. Woke up with my wife screaming and a glucagon pen in my arm. That was the day I became a CGM evangelist. And yes, carvedilol is the MVP here. Switched from metoprolol last year-zero scary lows since. If you’re on beta-blockers and not using tech to monitor? You’re not being brave. You’re being reckless. And no, ‘I check twice a day’ isn’t enough. Not anymore. Get with the program.
Zoe Bray
December 7, 2025 AT 17:48It is imperative to underscore that the pharmacodynamic interaction between insulin and beta-adrenergic antagonists constitutes a clinically significant, potentially life-threatening, drug-drug interaction. The suppression of adrenergic counterregulatory responses, particularly in the context of impaired hypoglycemia awareness, necessitates a paradigm shift in monitoring protocols. Continuous glucose monitoring is not merely an adjunct-it is a standard of care for this population. Furthermore, the selection of carvedilol over non-carvedilol beta-blockers is supported by robust evidence from the 2022 ADA/EASD consensus guidelines. Failure to implement these measures constitutes a deviation from accepted clinical practice.
Girish Padia
December 7, 2025 AT 21:32in india, we don't have cgms for most people. insulin is expensive. beta blockers? yeah, we get them cheap. but no one tells you this stuff. my uncle died from low sugar in sleep. no one knew. no alarm. no sweat even. just… gone. why do rich people get warnings and poor people get graves?
Saket Modi
December 8, 2025 AT 02:07why is everyone acting like this is news? i’ve been on propranolol + insulin for 8 years and i’ve had 3 seizures. i’m not mad, i’m just tired. nobody cares until it’s their kid. 🤷♂️