Medical Society Guidelines on Generic Drug Use: What Doctors Really Think
When your doctor writes a prescription, you might assume the pharmacy will fill it with the brand-name drug you recognize. But in most cases, they won’t. Over 90% of prescriptions in the U.S. are filled with generic drugs - not because patients ask for them, but because the system is built that way. Yet behind this quiet shift lies a deep divide among medical professionals. Some societies say generics are just as safe. Others warn that for certain drugs, even tiny differences can be dangerous.
What Medical Societies Actually Say About Generic Substitution
Medical societies don’t just comment on drugs - they set official positions that shape how doctors prescribe and how pharmacists substitute. These aren’t opinions. They’re policy statements backed by clinical data, reviewed by panels of specialists, and often tied to state laws. Take the American Academy of Neurology (AAN). They’ve been clear since at least 2023: don’t substitute generic versions of anticonvulsants without the prescriber’s approval. Why? Because epilepsy isn’t like high blood pressure. A 5% drop in blood concentration of a drug like levetiracetam or phenytoin can trigger a seizure. Even if the FDA says two versions are bioequivalent, neurologists see the real-world fallout - patients who were stable for years suddenly having breakthrough seizures after a pharmacy switch. On the other side, the American College of Physicians (ACP) supports generic substitution for most medications. Their stance is simple: if the FDA says it’s equivalent, then it is. And they’re right about the numbers. The FDA approves generics only after proving they deliver the same active ingredient, in the same strength, at the same rate as the brand. For antibiotics, statins, or blood pressure meds, the evidence is overwhelming: no difference in outcomes. Then there’s the National Comprehensive Cancer Network (NCCN). Their guidelines are unique. They don’t just accept generic oncology drugs - they actively list off-label uses for them. If a generic version of a chemotherapy drug is used for a cancer type not listed on its label, the NCCN may still classify it as a recommended treatment. That matters because Medicare uses NCCN data to decide what to pay for. So a doctor prescribing a generic drug off-label? It’s not just allowed - it’s covered.The Hidden Risk: Narrow Therapeutic Index Drugs
Not all drugs are created equal. Some have a wide safety margin. Take ibuprofen - you can take 400 mg or 600 mg and the difference is mostly in how fast your headache goes away. But drugs with a narrow therapeutic index (NTI) are different. The gap between a dose that works and one that harms is razor-thin. NTI drugs include:- Warfarin (blood thinner)
- Levothyroxine (thyroid hormone)
- Phenytoin, carbamazepine, valproate (anti-seizure meds)
- Lithium (for bipolar disorder)
- Cyclosporine (organ transplant rejection)
How Generic Drugs Get Their Names (And Why It Matters)
You’ve probably noticed that generic drugs have weird names. Lamotrigine. Esomeprazole. Levetiracetam. They don’t sound like the brand names - and that’s intentional. The American Medical Association’s USAN Council decides these names. Their job isn’t marketing. It’s safety. They avoid names that sound too similar to other drugs. Why? Because a pharmacist reading “Lamictal” and “Lamotrigine” might confuse them with “Lamivudine” - a totally different drug used for HIV. A mix-up like that could be deadly. The council uses “stems” to group drugs by class. For example, drugs ending in “-prazole” are proton-pump inhibitors. Those ending in “-pril” are ACE inhibitors. This helps doctors and pharmacists quickly recognize what a drug does - even if they’ve never heard the name before. But here’s the catch: the naming system isn’t perfect. Some newer drugs get names that are too similar. A 2023 AMA Journal of Ethics article warned that a poorly chosen name could make a company abandon a drug development project - not because it doesn’t work, but because the name looks too much like an existing one. That’s not just a naming problem. It’s a patient access problem.
Why Pharmacists Are Caught in the Middle
Pharmacists aren’t the ones deciding whether a generic is safe. But they’re the ones who have to dispense it. And they’re often the first to hear from patients who feel something’s off after a switch. “I had a patient come in crying because her seizure frequency doubled after her pharmacy switched her generic,” one pharmacist in Ohio told a national survey in 2023. “I checked the label - it was the same active ingredient. But she said, ‘This isn’t the same.’ And she was right. Her body knew.” State laws add to the confusion. In some places, pharmacists must notify the prescriber before substituting an NTI drug. In others, they can swap without telling anyone. And insurance companies? They often push for the cheapest option - even if it’s not the one the doctor intended. The result? A system where the patient gets the drug they’re supposed to get - but not always the one they need.The Economic Push Behind the Push for Generics
Let’s be honest: generics save money. A lot of it. In 2022, generics made up 90% of all prescriptions filled in the U.S. - but only 23% of total drug spending. That’s a massive savings. For Medicare, Medicaid, and private insurers, that’s billions of dollars a year. The Generic Pharmaceutical Industry Association (GPIA) - representing manufacturers and distributors - pushes hard for broader substitution. Their message is simple: generics are safe, effective, and cheaper. And statistically, they’re right. But medical societies aren’t just looking at cost. They’re looking at risk. For a patient with epilepsy, a $50 monthly savings isn’t worth the chance of a seizure. For someone on warfarin, the cost of a hospitalization from a bleed far outweighs the price difference. The real tension isn’t between brand and generic. It’s between system efficiency and individual safety.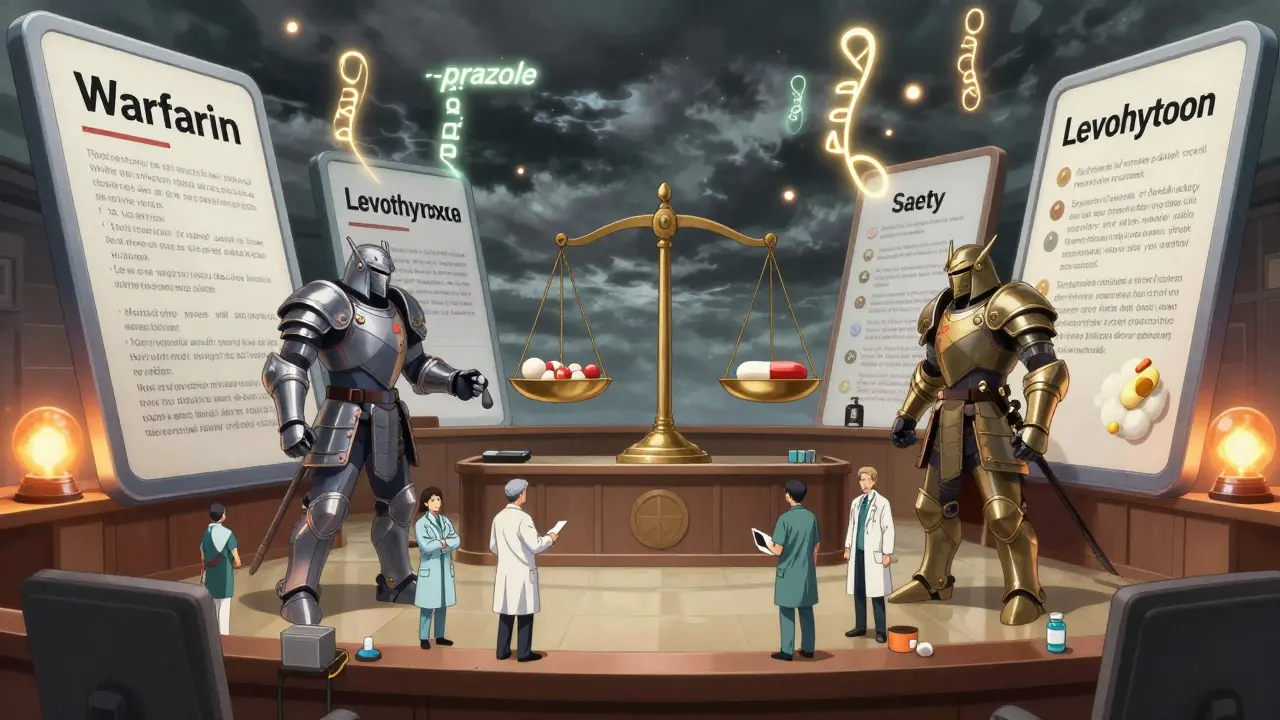
What Patients Should Do
You don’t need to be a doctor to protect yourself. Here’s what actually works:- Ask your doctor: “Is this drug on the NTI list?” If it is, ask them to write “Dispense as written” or “Do not substitute” on the prescription.
- If you’re on a drug like levothyroxine or warfarin, stick with the same generic brand if possible. If your pharmacy switches, ask them to tell you what changed.
- Keep a list of your medications - including the manufacturer name, not just the generic name. That way, if you switch pharmacies or doctors, you can say, “I’ve been taking the Teva version of levetiracetam.”
- Pay attention to how you feel after a refill. Fatigue, dizziness, mood changes, or new symptoms? Tell your doctor. It might not be the disease - it might be the pill.
Where This Is Headed
The FDA keeps updating its Orange Book, which rates drugs for therapeutic equivalence. More drugs are getting an “A” rating - meaning they’re interchangeable. That’s good for cost control. But medical societies aren’t backing down. The AAN isn’t going to change its stance on anticonvulsants. The NCCN will keep expanding off-label uses for generics in cancer care. And the USAN Council will keep refining names to prevent errors. The future isn’t about banning generics. It’s about smarter substitution. Not all drugs are equal. Not all patients are the same. And not all systems should treat them that way. The goal shouldn’t be to maximize substitution. It should be to maximize safety - without sacrificing affordability.Are generic drugs really as effective as brand-name drugs?
For most drugs, yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and bioequivalence as the brand. For antibiotics, blood pressure meds, or cholesterol drugs, studies show no difference in outcomes. But for drugs with a narrow therapeutic index - like warfarin, levothyroxine, or anti-seizure medications - even small differences in absorption can matter. That’s why some doctors avoid substitution in these cases.
Can a pharmacy switch my generic medication without telling me?
In most states, yes - unless your doctor writes “Dispense as written” or “Do not substitute.” For non-NTI drugs, pharmacists can switch brands freely. But for drugs like thyroid meds or seizure drugs, some states require prescriber approval. If you’re unsure, ask your pharmacist to confirm what version you’re getting and whether it’s the same as before.
Why do some doctors refuse to prescribe generics?
They don’t refuse generics outright. They refuse substitution for certain drugs - especially those with narrow therapeutic indices. Their concern isn’t that generics are inferior. It’s that even FDA-approved differences can cause real harm in sensitive patients. For example, a neurologist may have seen patients have seizures after a switch, even when the generic was technically equivalent. That’s why they document their clinical judgment in writing.
How do I know if my drug has a narrow therapeutic index?
Ask your doctor or pharmacist. Common NTI drugs include warfarin, levothyroxine, lithium, phenytoin, carbamazepine, cyclosporine, and digoxin. You can also check the FDA’s Orange Book - drugs with an “A” rating are considered interchangeable, but some may still carry special warnings for NTI use. If your drug is on the list, request that your prescription say “Do not substitute.”
Why do generic drugs have such strange names?
The American Medical Association’s USAN Council assigns generic names to help avoid confusion. They use “stems” - like “-prazole” for acid reducers or “-pril” for blood pressure drugs - so doctors can quickly identify the drug class. The goal is safety: a name that sounds too similar to another drug could lead to dangerous mix-ups. It’s not about marketing - it’s about preventing errors.






Comments
Joe Bartlett
December 16, 2025 AT 13:25Generics are fine for most stuff, but switch my thyroid med and I’m done. Saw a mate in the UK go from fine to exhausted after a swap. Docs need to stop treating patients like numbers.
Steven Lavoie
December 17, 2025 AT 12:41As someone who’s been on levothyroxine for 12 years, I can tell you: the brand matters. I switched to a generic once. Weight gain, brain fog, heart palpitations. Went back to Synthroid and everything normalized. FDA bioequivalence doesn’t mean biological equivalence. There’s a difference.
Naomi Lopez
December 18, 2025 AT 06:21Ugh. I had a neurologist tell me my generic lamotrigine was ‘just as good.’ Two weeks later I had my first grand mal in five years. Now I hand-write ‘DO NOT SUBSTITUTE’ on every script. No one listens until someone gets hurt.
Salome Perez
December 19, 2025 AT 09:00The real tragedy isn’t the cost savings-it’s the erasure of clinical nuance. Medicine isn’t a spreadsheet. A 10% fluctuation in warfarin levels isn’t ‘statistically insignificant’ to someone who nearly bled out. The system rewards efficiency, not individualized care. And patients pay the price in fear, hospital visits, and lost trust.
Pharmacists aren’t villains-they’re trapped between insurers, regulators, and physicians who don’t always speak up. But we need policy that honors biological variability, not just chemical equivalence.
BETH VON KAUFFMANN
December 20, 2025 AT 23:45NTI drugs? Please. The FDA’s 80–125% bioequivalence window is a joke. That’s a 45% swing! If you were manufacturing a rocket engine, you’d be sued for tolerances that wide. But for human biology? Meh. Let’s just save a buck.
And don’t get me started on the naming conventions. ‘Esomeprazole’? Sounds like a failed sci-fi villain. Meanwhile, ‘Nexium’ is branded like a luxury sneaker. Capitalism at its finest.
Victoria Rogers
December 22, 2025 AT 02:33They’re all just part of the pharmaceutical cartel. Brand names are overpriced because they own the FDA. Generics? Same exact pills, just cheaper. But they make you think there’s a difference so you’ll keep paying more. Wake up. It’s all profit.
Pawan Chaudhary
December 22, 2025 AT 21:56India makes most generics and they’re super safe! My cousin takes them for diabetes and hypertension-no issues. Maybe US doctors are too cautious?
Virginia Seitz
December 24, 2025 AT 18:04My pharmacist switched my levetiracetam and I cried. 😭 Not because I’m dramatic-because I almost lost my job from seizures. Now I keep the box. Always. #DontSwitchMyMed
Peter Ronai
December 26, 2025 AT 13:50Oh please. You’re all being manipulated. The AAN’s stance? Pure fearmongering. The NCCN supports generics because they’re cost-effective. The truth? Big Pharma bribes doctors to scare you into paying $500 for a pill that costs $2 to make. Wake up, sheeple.
amanda s
December 27, 2025 AT 01:05My mom died because they switched her warfarin brand. No warning. No consent. Just a different pill. And now they want to make this standard? This isn’t healthcare. It’s mass murder with a clipboard.
Evelyn Vélez Mejía
December 27, 2025 AT 15:29What we’re witnessing isn’t a debate over pharmacology-it’s a collision between two ethical paradigms: utilitarian efficiency versus individualized bioethics. The system optimizes for population-level outcomes, but medicine, at its core, is the care of the singular. When we reduce a human being to a data point in a cost-benefit analysis, we don’t just risk harm-we abandon the moral foundation of the profession.
Generics are not the enemy. The abstraction of care is.
Michael Whitaker
December 28, 2025 AT 03:46It’s fascinating how laypeople romanticize the ‘patient experience’ while ignoring the rigorous, peer-reviewed pharmacokinetic data that underpins FDA approval. The notion that ‘my body knows’ is not science-it’s anecdotal confirmation bias. If you’re experiencing adverse effects, it’s more likely noncompliance, drug interactions, or psychosomatic response than bioequivalence failure.
And for the record, the USAN Council is not some rogue body-it’s a globally recognized authority. The naming conventions are designed to prevent errors across languages, scripts, and systems. To dismiss them as ‘weird’ is to misunderstand the entire architecture of clinical safety.
Chris Van Horn
December 28, 2025 AT 13:33My neurologist told me the same thing: ‘It’s the same chemical.’ But when I switched generics, I had three seizures in one week. I called the pharmacy. They said, ‘We’re just following the law.’ So now I pay $200 out of pocket for the brand. Because the system is broken. And no one in charge cares.
They’re not protecting patients. They’re protecting profits. And if you think this isn’t happening to you, you’re next.
Jonathan Morris
December 30, 2025 AT 06:02Did you know the FDA allows generics to be made in China? And that the same facility that made the tainted heparin in 2008 still supplies 80% of our generics? No one talks about this. But I’ve seen the reports. The ‘bioequivalence’ tests? They’re outdated. They test blood levels at 24 hours-but what about peak absorption? What about metabolites? They’re not measuring what matters.
This isn’t about cost. It’s about control. And someone’s watching. And they’re not letting you know.