Prior Authorization Requirements for Medications Explained: What You Need to Know

If you’ve ever been told your doctor can’t fill your prescription right away - even though it’s been prescribed - you’ve run into prior authorization. It’s not a glitch. It’s not a mistake. It’s a standard step in how most health insurance plans in the U.S. control costs. And if you’re on a long-term medication, especially a high-cost one, you’ll likely face it more than once.
What Is Prior Authorization?
Prior authorization - sometimes called pre-authorization or prior auth - is when your insurance company requires approval before they’ll pay for a specific medication. Your doctor doesn’t just write a prescription and hand it to the pharmacy. They have to send paperwork to your insurer first, explaining why you need that drug and why cheaper options won’t work.
This isn’t about slowing you down for no reason. Insurance companies use prior authorization to make sure you’re getting the right drug for your condition, at the right price. For example, if there’s a generic version of your medication that works just as well, they’ll want you to try that first. Or if a drug is expensive and has serious side effects, they’ll want proof it’s truly necessary.
Medicare Part D calls this a “coverage determination.” Blue Shield of California and Cigna use similar terms. The goal? To balance safety, effectiveness, and cost. According to the Academy of Managed Care Pharmacy, prior authorization helps ensure medications are “safe, effective for their condition, and provide the greatest value.”
Which Medications Need Prior Authorization?
Not every drug needs approval. But if your prescription falls into one of these categories, you’re likely to hit a wall at the pharmacy:
- Brand-name drugs with generic alternatives - If a cheaper, equally effective version exists, insurers will make you try it first.
- High-cost medications - Think cancer drugs, specialty biologics, or treatments for rare conditions. These can cost thousands per month.
- Drugs with strict usage rules - Some meds are only approved for certain conditions. For example, a drug for rheumatoid arthritis might not be covered if your doctor prescribes it for back pain.
- Medications with dangerous interactions - If you’re on multiple prescriptions, your insurer might want to check for risky combinations.
- Drugs with abuse potential - Opioids, stimulants, and certain sedatives often require extra scrutiny.
It’s not random. Each insurance plan has a list called a “formulary” - a catalog of covered drugs. If your drug isn’t on that list, or has restrictions, prior auth kicks in. You can check your plan’s formulary online or call customer service. Most insurers, like Blue Shield of California, offer tools like “Price Check My Rx” to see if a drug needs approval before you even leave the doctor’s office.
Who Starts the Process?
Your doctor or their staff handles the paperwork. They fill out a form - often online or via fax - with details about your diagnosis, medical history, and why the requested drug is necessary. They might need to show that you’ve already tried other treatments without success.
For off-label uses - when a drug is prescribed for something not officially approved by the FDA - the bar is even higher. Your provider may need to submit medical studies or clinical evidence supporting the use. Some insurers even assign a pharmacist to review the literature before approving it.
And here’s something many patients don’t realize: some drugs can only be prescribed by specialists. Chemotherapy drugs, for example, are often restricted to oncologists. If your primary care doctor prescribes one, the request will be denied unless a specialist signs off.
How Long Does It Take?
The wait time varies. For routine requests, it can take 2 to 5 business days. If your condition is urgent - like a flare-up of a chronic illness or risk of hospitalization - you can ask for an “urgent prior authorization.” In those cases, insurers are required to respond within 24 to 72 hours.
But approval isn’t permanent. Most prior authorizations last for a set period - often 3 to 12 months. After that, your doctor has to reapply. If you refill your prescription after the authorization expires, the pharmacy will decline it. That’s why it’s important to keep track of expiration dates.
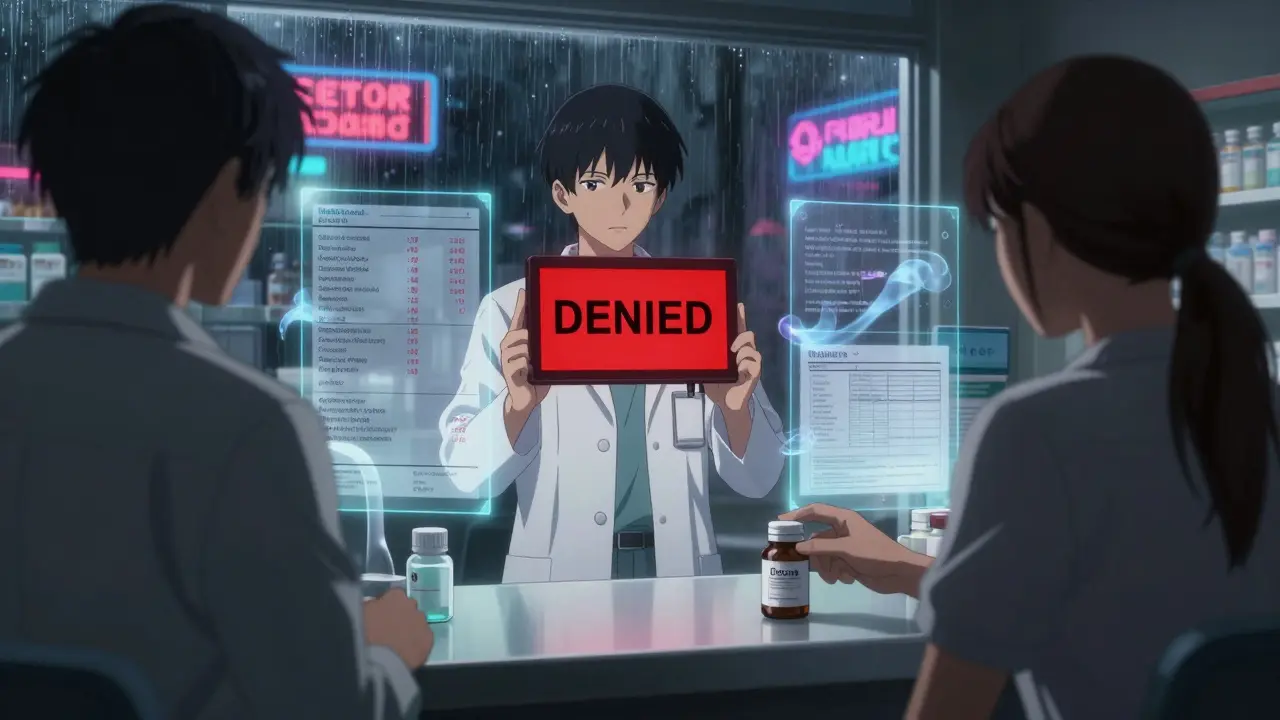
What Happens If It’s Denied?
Denials happen. Sometimes it’s because the paperwork was incomplete. Other times, the insurer just doesn’t think the drug is medically necessary.
If your request is denied, your doctor can file an appeal. They’ll submit additional medical records, lab results, or letters explaining why the drug is essential. You can also request a peer-to-peer review - where your doctor talks directly to a medical reviewer from the insurance company.
Don’t give up. Many appeals are successful, especially when supported by strong clinical evidence. Medicare and most private plans have formal appeal processes. You have the right to challenge a denial.
What Can You Do as a Patient?
You’re not powerless in this process. Here’s what you can do:
- Ask your doctor before the appointment - “Will this medication need prior authorization?” If yes, ask them to start the request right away.
- Check your plan’s formulary - Log into your insurer’s website or call them. Know what’s covered and what’s not.
- Ask about alternatives - If your drug requires prior auth, ask if there’s a similar drug on the formulary that doesn’t. Sometimes a small switch saves weeks of waiting.
- Follow up - Don’t assume your doctor’s office handled it. Call them a few days later to confirm the request was sent.
- Pay out-of-pocket temporarily - If you can’t wait, pay for the medication yourself and submit a claim for reimbursement after approval. GoodRx and other services can help you find cash prices that are sometimes cheaper than your copay.
Remember: you’re responsible for knowing your coverage. The Mayo Clinic says patients should always confirm whether a prescribed medication is covered before leaving the office.

When Is Prior Authorization Not Required?
There are exceptions. If you’re having a medical emergency, your insurer must cover the medication without prior authorization. That includes ER visits, urgent care, or sudden health crises.
Also, if you’re already taking a drug and your insurance plan changes - say, you switch from one Medicare Part D plan to another - you may get a temporary 30-day supply while your prior auth is processed. This is called a “transition policy.”
Why Does This System Exist?
It’s not perfect. Doctors complain it wastes time. Patients get frustrated. But the system exists because drug prices in the U.S. are sky-high. A single course of some specialty medications can cost over $100,000 a year. Without checks, insurers would be overwhelmed.
Prior authorization isn’t about denying care. It’s about ensuring care is appropriate. For example, if a patient with mild depression is prescribed a $6,000/month antidepressant when a $10 generic works just as well, the insurer steps in. That’s not cruelty - it’s cost control with clinical oversight.
The American Medical Association says doctors wish patients understood this: prior auth is a tactic insurers use to control costs - but it’s also meant to prevent unnecessary or unsafe prescribing.
What’s Changing?
There’s growing pressure to simplify the process. Some states have passed laws limiting how long insurers can take to respond. Medicare is testing faster electronic systems. Pharmacies are pushing for real-time prior auth checks at the point of sale.
But for now, the system remains complex. The key is to stay informed, stay involved, and don’t let a delay stop you from getting the care you need.
Does prior authorization mean my insurance won’t cover my medication?
No. Prior authorization means your insurance needs more information before approving coverage. It’s a gate, not a wall. If your doctor provides the right documentation showing medical necessity, your medication will be covered.
Can I get my medication without prior authorization?
Only if your drug doesn’t require it. If your plan requires prior auth for that medication, the pharmacy won’t fill it until approval is granted. You can pay cash upfront, but you’ll need to submit a claim later for reimbursement if approval comes through.
How do I know if my drug needs prior authorization?
Check your insurance plan’s formulary online, use their Price Check tool, or call customer service. Your doctor’s office should also let you know before prescribing. When in doubt, ask.
Why does my doctor have to do all the paperwork?
Because they’re the one who understands your medical history and can prove the medication is necessary. Insurance companies require clinical justification - not just a prescription. Your doctor’s signature confirms the request is accurate and truthful.
Can I switch to a different medication to avoid prior authorization?
Yes, and often you should. Many drugs in the same class work similarly. Ask your doctor if there’s an alternative on your plan’s formulary that doesn’t require prior auth. It could save you weeks of waiting - and possibly money.






Comments
Sharon Biggins
January 24, 2026 AT 22:36i just had to wait 3 weeks for my lupus med to get approved... my doctor’s office said they submitted it right away but the insurer kept asking for ‘more info’ like what info?? i already gave them 12 pages of records. i’m so tired of this system.
John McGuirk
January 26, 2026 AT 13:21this is all just a cover for big pharma and insurers to keep prices high. they want you to suffer so they can sell you the ‘premium’ version later. they don’t care if you die waiting. it’s profit over people. always.
Michael Camilleri
January 26, 2026 AT 23:24people act like this is some new horror show but its just capitalism doing its job. you want cheap meds? then accept that someone has to gatekeep. doctors aren’t saints and insurers aren’t villains. we’re all just cogs. the real problem? you think you deserve something for free. you don’t. you pay for it one way or another. stop pretending.
lorraine england
January 27, 2026 AT 14:47my mom got denied for her heart med last year and i helped her appeal. we sent in her echocardiogram results, her doctor’s letter, and even a note from her cardiologist saying she’d be hospitalized without it. they approved it in 4 days. don’t give up. it’s annoying but it’s not impossible. you got this 💪
Darren Links
January 29, 2026 AT 05:27if you’re not american you have no idea how broken this is. in europe they just give you the drug. here we have to beg for our own prescriptions. i mean… we pay for insurance right? so why does it feel like we’re asking for charity?
Kevin Waters
January 29, 2026 AT 23:03one thing that helped me: i started using GoodRx before every refill. sometimes the cash price is lower than my copay after prior auth. i also set phone reminders for when my auth expires. i’ve saved myself 3 emergency pharmacy trips by just staying organized. small habits make a big difference.
Kat Peterson
January 30, 2026 AT 22:23ok but like… imagine being a doctor and having to fill out 17 forms for ONE drug?? 😭 i swear if i had to do one more prior auth i’d quit medicine and move to a cave. this is not healthcare. this is bureaucratic hell with a side of anxiety.
Himanshu Singh
February 1, 2026 AT 15:52the system is flawed but the intention is not evil. we need checks because drugs are expensive and misuse is real. imagine if everyone got the newest $10k pill for mild headaches. the key is balance. doctors and insurers should work together, not against each other. patience and persistence help. 🙏
Jamie Hooper
February 1, 2026 AT 17:53they say its for cost control but honestly its just a way to make patients feel powerless. i had to wait 18 days for my ADHD med and my boss thought i was slacking off. meanwhile the insurance company made 3 million in profit last quarter. so yeah. thanks for nothing.