Quality concerns: when clinicians question generic manufacturing

When a doctor prescribes a generic drug, most patients assume it’s just as safe and effective as the brand-name version. After all, the FDA says so. But behind the scenes, many clinicians are starting to ask harder questions-especially when the same pill comes from a factory in India versus one in Ohio. And it’s not just about price anymore. It’s about whether the system is still working.
What’s really in that pill?
Generic drugs aren’t copies. They’re supposed to be identical in active ingredient, strength, and how the body absorbs them. But here’s the catch: the active ingredient might be made in one country, mixed with fillers in another, coated in a third, and packaged in a fourth. The label? Just one company name. You have no idea which factories actually touched your medicine. That’s not a conspiracy. It’s how the system works. The FDA requires bioequivalence-meaning the drug must deliver the same amount of active ingredient at the same rate as the brand. But bioequivalence doesn’t guarantee consistency across batches. It doesn’t catch impurities. It doesn’t stop a factory from cutting corners when the profit margin is razor-thin.The numbers don’t lie
A 2023 study from Ohio State University looked at over 200 million adverse event reports in the FDA’s database. They matched generic drugs made in the U.S. with identical drugs made in India-and found something startling. Indian-made generics were linked to 54% more severe adverse events: hospitalizations, disabilities, even deaths. And it wasn’t random. The gap got wider for older, cheaper generics-the ones that have been on the market for years and have seen the most price pressure. Professor Robert S. Gray, who led the study, put it plainly: “As drugs get cheaper and cheaper and the competition gets more intense to hold down costs, operations and supply chain issues can compromise drug quality.” That’s not a theory. It’s data.Inspections that don’t inspect
The FDA inspects U.S. drug factories without warning. That’s a deterrent. If you’re cutting corners, you can’t just clean up the day before they show up. Overseas? Not so much. Inspections are scheduled months in advance. Manufacturers know exactly when they’re coming. They can stage the facility, hide problems, delay shipments, or even shut down lines temporarily. It’s like letting a restaurant know the health inspector is coming next Tuesday-do you think they’d clean the kitchen the night before? Of course they would. The FDA has over 1,300 staff dedicated to drug quality. But they can’t be everywhere. And when 86% of active pharmaceutical ingredients come from outside the U.S.-mostly from India and China-the math doesn’t add up.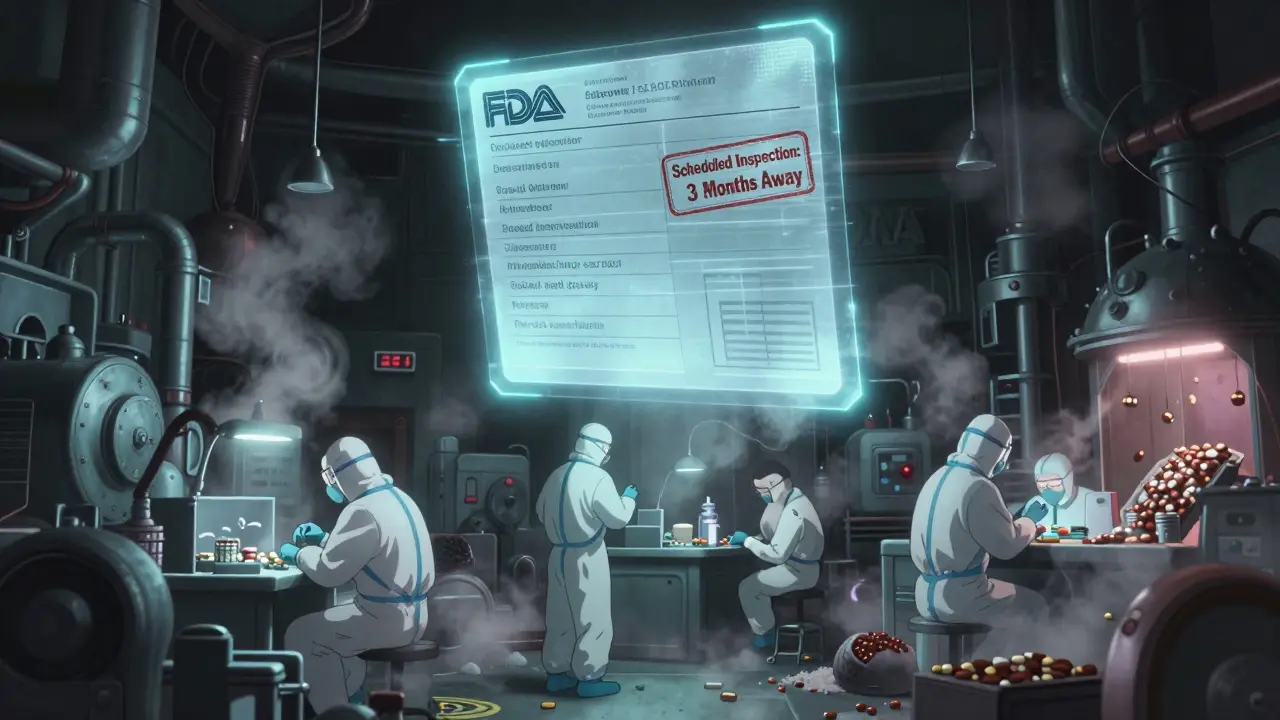
Why older generics are the biggest risk
Newer generics? They’re often made with modern equipment. But older ones? Many were approved decades ago. The manufacturing tech hasn’t changed. The price has dropped. The competition is brutal. Companies that once made a decent profit now survive on pennies per pill. Duke University researchers found that these older, low-margin generics are the leading cause of drug shortages. Why? Because when a machine breaks down or a batch fails quality control, there’s no profit left to fix it. No incentive to upgrade. No budget for real quality control. So the factory keeps shipping-until it doesn’t. Clinicians see the fallout. A patient on a generic blood thinner suddenly has a stroke. A cancer patient’s chemo is delayed because the generic version wasn’t available. A diabetic’s insulin doesn’t work the same way. These aren’t rare cases. They’re symptoms of a broken system.Is the FDA’s approval enough?
The FDA insists the system works. And technically, they’re right. Most generics are fine. But “most” isn’t good enough when someone’s life is on the line. The agency approves drugs based on lab data submitted by manufacturers-not real-world outcomes. And they rely on manufacturers to report problems. That’s like trusting a car company to self-report whether their brakes fail. Some do. Others don’t. The FDA doesn’t test every batch. They don’t even test every factory every year. Meanwhile, countries like Germany and Sweden have stricter post-market surveillance. They track outcomes, not just paperwork. And guess what? Their doctors trust generics more.Can advanced manufacturing fix this?
There’s a solution hiding in plain sight: advanced manufacturing technologies (AMTs). Things like continuous production, real-time monitoring, and automated quality checks. These aren’t sci-fi. They’re already being used in over 80% of U.S.-made drugs. They reduce waste. They catch errors before a batch leaves the plant. They make production more reliable. And here’s the kicker: once you invest in them, the per-unit cost drops. It’s not more expensive-it’s smarter. But most overseas manufacturers won’t adopt them. Why? Because their business model is built on low cost, not high quality. They compete on price, not precision. And if you’re making a pill for 2 cents, you can’t afford $5 million in new equipment.
What clinicians are doing about it
Some doctors are starting to ask patients: “Where was this made?” Not to scare them-but to understand. If a patient’s condition suddenly worsens after switching to a new generic, they’re looking at the source. Pharmacists are pushing back too. Some hospitals now require proof of quality certification before stocking a generic. Others refuse to carry certain brands entirely. One oncology center in Chicago stopped using a specific generic chemo drug after three patients had unexpected reactions-all traced to the same Indian manufacturer. Dr. Iyer, a pharmacist and researcher, says the answer isn’t more regulation-it’s market pressure. “Procurers can incentivize quality by ensuring they only purchase from those who can demonstrate quality assurance.” In other words: pay more for better. Let the market reward the good manufacturers.Domestic production isn’t a luxury-it’s a safety net
The University of Wisconsin School of Pharmacy put it simply: “If we have more generic manufacturing happening domestically, we would ideally have fewer quality concerns, fewer shortages, and a more stable supply chain.” It’s not about nationalism. It’s about control. When a factory is in the U.S., you can visit. You can inspect. You can audit. You can hold someone accountable. When a factory is on the other side of the world, you’re relying on documents, photos, and promises. And when geopolitical tensions rise-like trade wars, shipping blockades, or pandemics-those supply chains snap. We’ve seen it. During COVID, we ran out of basic antibiotics because the API came from China. And no one could get it.The bottom line
Generic drugs saved billions. They made medicine affordable. But affordability shouldn’t mean acceptability. We can’t keep pretending that a pill made in five different countries, inspected once every three years, and priced at 90% off the brand is just as safe. Clinicians aren’t against generics. They’re against the system that lets quality slip through the cracks. They’re asking for transparency. For inspections that aren’t scheduled. For manufacturers to be held to the same standard-no matter where they are. The FDA could fix this tomorrow by requiring country-of-origin labeling on every generic drug. Let patients and doctors choose. Let the market reward quality. Let the bad actors lose business. Because when a doctor looks at a prescription and wonders if the pill will work-or if it’ll hurt-they shouldn’t have to guess.Are generic drugs really as good as brand-name drugs?
Most generics work just fine. But not all. The FDA requires them to match brand-name drugs in active ingredient and absorption rate, but not in manufacturing quality, purity, or consistency across batches. Studies show that generics made overseas-especially older, low-cost ones-have higher rates of severe side effects compared to those made in the U.S.
Why do some generic drugs cause more side effects than others?
It’s often about manufacturing practices. Older generics face intense price pressure, leading manufacturers to cut costs on quality control, use outdated equipment, or source cheaper-but riskier-raw materials. A 2023 study found Indian-made generics had 54% more severe adverse events than U.S.-made versions of the same drug, especially for older medications.
Does the FDA inspect foreign drug factories the same way as U.S. ones?
No. The FDA conducts unannounced inspections in U.S. facilities but schedules inspections months in advance overseas. This gives manufacturers time to clean up, hide issues, or temporarily shut down problem areas. Experts say this undermines the ability to catch real quality problems.
Can advanced manufacturing improve generic drug quality?
Yes. Technologies like continuous manufacturing and real-time monitoring catch errors before a batch is released. Over 80% of U.S.-made drugs now use these methods, leading to fewer defects and shortages. But most overseas manufacturers won’t invest because their low-cost model doesn’t allow it.
Should I avoid generic drugs made overseas?
Not necessarily. Many overseas-made generics are safe and effective. But if you’re on a critical medication-like blood thinners, epilepsy drugs, or insulin-and you notice a change in how you feel after a refill, ask your pharmacist where it was made. Some hospitals and clinics now track this. Transparency helps patients and doctors make better choices.
Is there a push to bring generic manufacturing back to the U.S.?
Yes. Experts from the University of Wisconsin and Duke-Margolis Center argue that domestic production reduces shortages and improves quality control. While initial investment is high, advanced manufacturing lowers long-term costs. Some lawmakers are proposing incentives to rebuild U.S. generic drug capacity-but progress is slow.





Comments
clarissa sulio
February 3, 2026 AT 03:04Let’s be real-why are we still letting foreign factories make our life-saving pills? The FDA can’t even inspect them properly, and we’re supposed to trust a label that says ‘Made in India’ like it’s a guarantee? I don’t care how cheap it is-if my grandma’s blood thinner fails because some factory skipped a quality check, that’s not a savings, that’s a crime.
Bridget Molokomme
February 3, 2026 AT 06:38Oh wow, so now we’re blaming India for everything? Funny how the same people who scream about outsourcing jobs are fine with outsourcing their prescriptions. The real problem? We stopped investing in domestic manufacturing because we got lazy and wanted $3 pills. Now we’re shocked when the system crumbles? Classic.
Vatsal Srivastava
February 4, 2026 AT 10:16You think US made is better? Ha. Most US generics are just repackaged Indian API with fancy labels. The system is broken everywhere. You just like your own government’s lies more.
Brittany Marioni
February 4, 2026 AT 14:38Can we please, please, PLEASE start labeling the country of origin on every generic pill? Not just for transparency-but so that people who need stability-like those on anticoagulants, epilepsy meds, or insulin-can make informed choices? It’s not about fear-it’s about agency. And if we’re going to demand accountability from pharmaceutical companies, let’s start by giving patients the facts.
Monica Slypig
February 5, 2026 AT 23:25Why are we even debating this? The FDA is a joke. They approve drugs based on paperwork from companies that bribe inspectors. And now we’re surprised when people die? I’ve seen too many patients crash after switching to a new generic. No one checks. No one cares. Until it’s your kid on a ventilator.
Becky M.
February 6, 2026 AT 10:09i know this is a hard topic... but i just want to say... maybe we need to think about this not as us vs them... but as a global system that needs fixing... i mean, yes, indian factories have issues... but so do some u.s. ones... maybe instead of blaming countries... we should push for global standards? like... real audits... not scheduled ones... and maybe... funding for modern tech everywhere?
jay patel
February 7, 2026 AT 20:53Look, I get the fear. I’ve worked in pharma logistics for 15 years. I’ve seen factories in Gujarat that run like Swiss clocks. And I’ve seen others where the lab coats are dirty and the temperature logs are faked. The problem isn’t India. The problem is the race to the bottom. When a pill costs two cents, no one can afford to do it right. The solution isn’t nationalism-it’s fair pricing. Pay more for quality. Reward the good factories. Punish the bad ones. Not by banning imports-but by making ethics profitable.
Ansley Mayson
February 9, 2026 AT 12:40So what? People die every day. This isn’t new. The FDA approves 99% of generics. The rest are outliers. Stop sensationalizing. You want better drugs? Pay more. Simple.
phara don
February 10, 2026 AT 00:57Interesting. So if advanced manufacturing reduces costs long-term, why aren’t more overseas plants adopting it? Is it just capital? Or is it that they’re locked into old contracts with distributors who only care about lowest bid? Maybe we need a tiered labeling system-like energy ratings for appliances? Gold/Silver/Bronze for quality?
Hannah Gliane
February 10, 2026 AT 01:58OMG I can’t believe you’re still letting your grandma take these death pills 😭 I literally cried reading this. My cousin had a seizure because of a generic from China. We need to ban ALL foreign generics. Like, NOW. And put everyone who makes them in jail. 💀🩸 #DrugSafety #MakePillsGreatAgain
Murarikar Satishwar
February 11, 2026 AT 19:57There’s a quiet truth here that no one wants to say out loud: the system works fine for most people most of the time. But when it fails, it fails catastrophically. That’s why we need traceability-not just country of origin, but batch-level tracking. Every pill should have a digital passport. That’s not expensive. It’s already possible. And if we demand it, manufacturers will build it. The market doesn’t need to be protected-it needs to be informed.