Bactrim and Blood Thinners: Risks, Interactions, and What to Watch For
When you take Bactrim, a combination antibiotic made of sulfamethoxazole and trimethoprim, commonly prescribed for urinary tract infections, bronchitis, and other bacterial infections, and you’re also on a blood thinner, a medication like warfarin, apixaban, or rivaroxaban used to prevent dangerous clots, you’re walking into a hidden risk zone. These two types of drugs don’t just coexist—they can amplify each other’s effects in ways that aren’t obvious until it’s too late. The problem isn’t just theoretical. Studies show that patients on warfarin who start Bactrim have a 2- to 3-fold increase in bleeding events, including nosebleeds, bruising, and even internal bleeding. This isn’t a rare fluke—it’s a well-documented interaction that doctors and patients often miss.
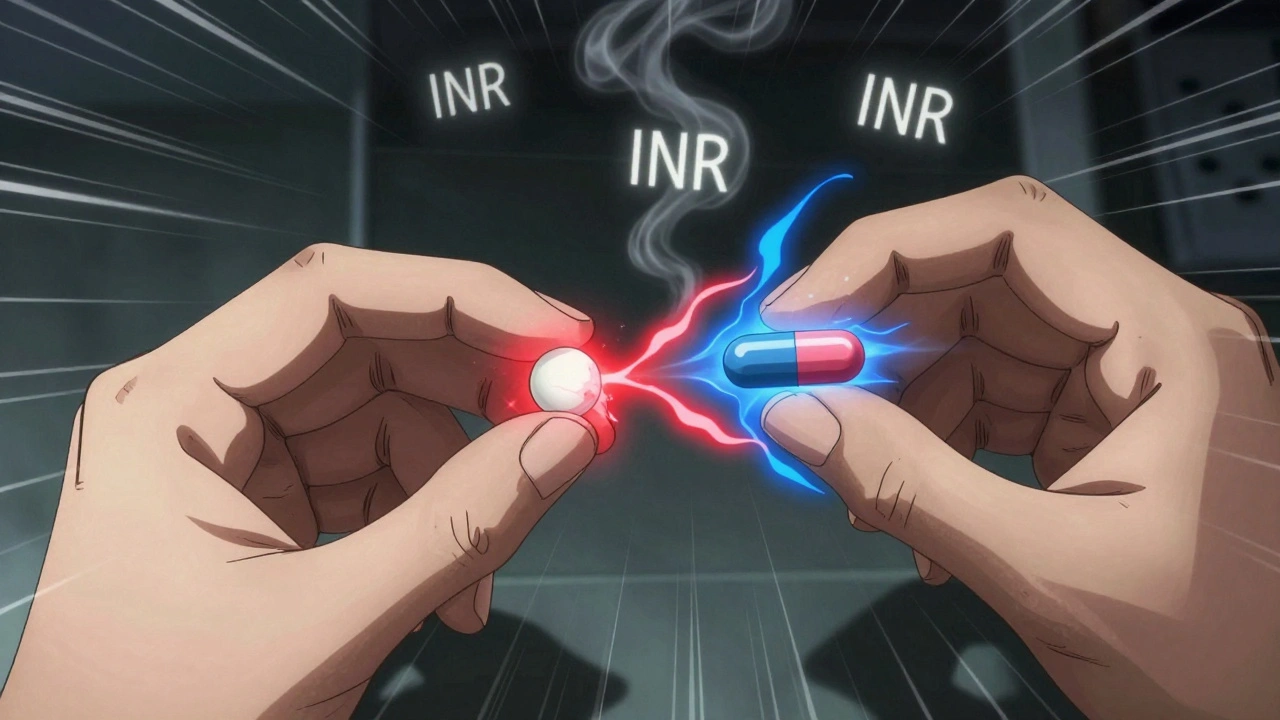
Why does this happen? Bactrim interferes with how your liver breaks down warfarin, causing the blood thinner to build up in your system. It also reduces vitamin K production in your gut, which is critical for clotting. The result? Your blood thins more than intended. Even if your INR (the test that measures blood thinning) was stable for months, adding Bactrim can send it soaring in just a few days. People over 65, those with kidney problems, or anyone already on multiple medications are at highest risk. And it’s not just warfarin—newer blood thinners like apixaban and rivaroxaban can also be affected, though the data is still emerging. You can’t assume a "newer" drug is safer in this case. If you’re on any anticoagulant and your doctor prescribes Bactrim, ask: "What’s the plan to monitor this?" Don’t wait for symptoms like unusual bruising, blood in urine or stool, or dizziness to act.
Some patients think switching to a different antibiotic solves the problem, but not all alternatives are safer. Clindamycin, for example, carries its own risks like C. difficile infection. Amoxicillin might be a better choice for some, but only if the infection allows it. The real solution isn’t just swapping drugs—it’s communication. Keep a list of every medication you take, including over-the-counter pills and supplements. Share it with every provider, even if they don’t ask. Use a lab monitoring calendar, a simple tool to track blood tests like INR when you start or stop a new drug to stay ahead of changes. If you’ve ever had a bad reaction to a medication, write it down. That note could save your life.
What you’ll find below are real, practical guides from people who’ve been there—how to spot early signs of bleeding, how to talk to your pharmacist about drug clashes, what to do if you miss a dose, and how to safely manage multiple prescriptions without panic. These aren’t theory pieces. They’re the kind of advice you wish you’d found before your next prescription came in.
Trimethoprim-Sulfamethoxazole and Warfarin: Why INR Rises and How to Stay Safe
Trimethoprim-sulfamethoxazole can cause dangerous INR spikes in people taking warfarin, increasing bleeding risk. Learn why this happens, who’s most at risk, and how to stay safe with proper monitoring and alternatives.