Hyperkalemia — when potassium gets too high and what to do
High potassium sounds harmless, but it can stop your heart. If you or someone you care for has kidney problems, takes certain meds, or uses salt substitutes, this is one thing you should know how to spot and act on fast.
What hyperkalemia looks like and what causes it
Hyperkalemia means blood potassium is higher than normal. Mild cases may cause tiredness, muscle weakness, or tingling. More serious rises bring palpitations, chest pain, fainting, or sudden weakness — and those need emergency care. Kidneys do most of the work removing potassium, so chronic kidney disease is the single biggest risk.
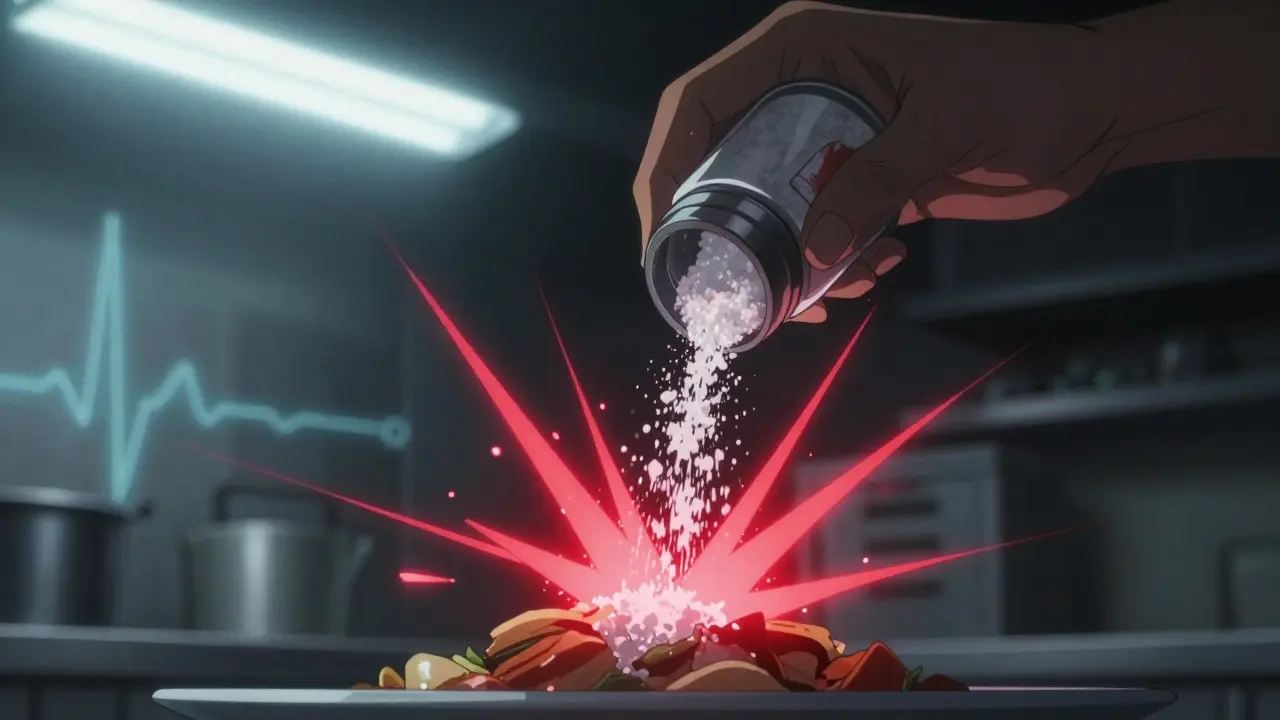
Other common causes: certain drugs (ACE inhibitors, ARBs, spironolactone and other potassium-sparing diuretics, trimethoprim, some NSAIDs), large potassium supplements, rapid tissue breakdown (severe injury, rhabdomyolysis), acidosis, and dehydration. Even swapping table salt for potassium-based salt can push levels up if your kidneys are weak.
Recognize and respond — tests and immediate steps
If you suspect high potassium, the quick tests are a blood potassium level and an ECG. The ECG often shows peaked T waves, a widened QRS, or dangerous irregular rhythms. If ECG changes or very high potassium appear, get emergency care.
In hospital, doctors use treatments that protect the heart and move potassium out of the blood. Calcium gluconate stabilizes the heart right away. Insulin with glucose shifts potassium into cells fast. Nebulized salbutamol and intravenous sodium bicarbonate help in specific cases. For longer-term removal, diuretics, potassium binders (patiromer, sodium zirconium cyclosilicate) or dialysis are options depending on the situation.
If you’re at home and suspect mild symptoms, call your doctor for same-day testing. If you have chest pain, sudden fainting, severe weakness, or a history of kidney failure, call emergency services immediately.
Small habits help reduce risk: keep a current meds list, check kidney function and potassium when starting drugs like spironolactone or ACE inhibitors, and avoid potassium supplements unless a clinician prescribes them.
Avoid sudden diet panic, but be smart about foods if you’re at risk. High-potassium items include bananas, potatoes, tomatoes, oranges, spinach, and many salt substitutes. Your clinician can give tailored limits based on lab results.
If you use medications that raise potassium, ask for a monitoring plan: frequency of blood tests, warning signs, and who to call. Early detection is the safest path — hyperkalemia can be managed well when treated fast and sensibly.
Salt Substitutes and ACE Inhibitors or ARBs: The Hidden Potassium Danger
Salt substitutes with potassium chloride can cause dangerous potassium buildup in people taking ACE inhibitors or ARBs, leading to life-threatening hyperkalemia. Learn who’s at risk and what to do instead.
Managing Spironolactone-Induced Hyperkalemia
Managing Spironolactone-induced hyperkalemia can be quite challenging for some individuals. In my experience, I've found that closely monitoring potassium levels and adjusting the dosage of Spironolactone accordingly is crucial. Additionally, it's essential to maintain a low-potassium diet and stay well-hydrated to help prevent complications. Consulting with a healthcare professional regularly and promptly reporting any symptoms of hyperkalemia, such as muscle weakness or irregular heartbeats, can make all the difference in managing this condition effectively. Overall, taking a proactive approach to managing Spironolactone-induced hyperkalemia is key to ensuring optimal health and well-being.