Vaginal infections: easy-to-follow signs and steps
Vaginal infections are common and usually treatable, but they can be confusing. Not every itch or discharge means the same thing. This page helps you spot the likely cause, try safe first steps at home, and know when to get a proper exam or prescription.
Recognize the type
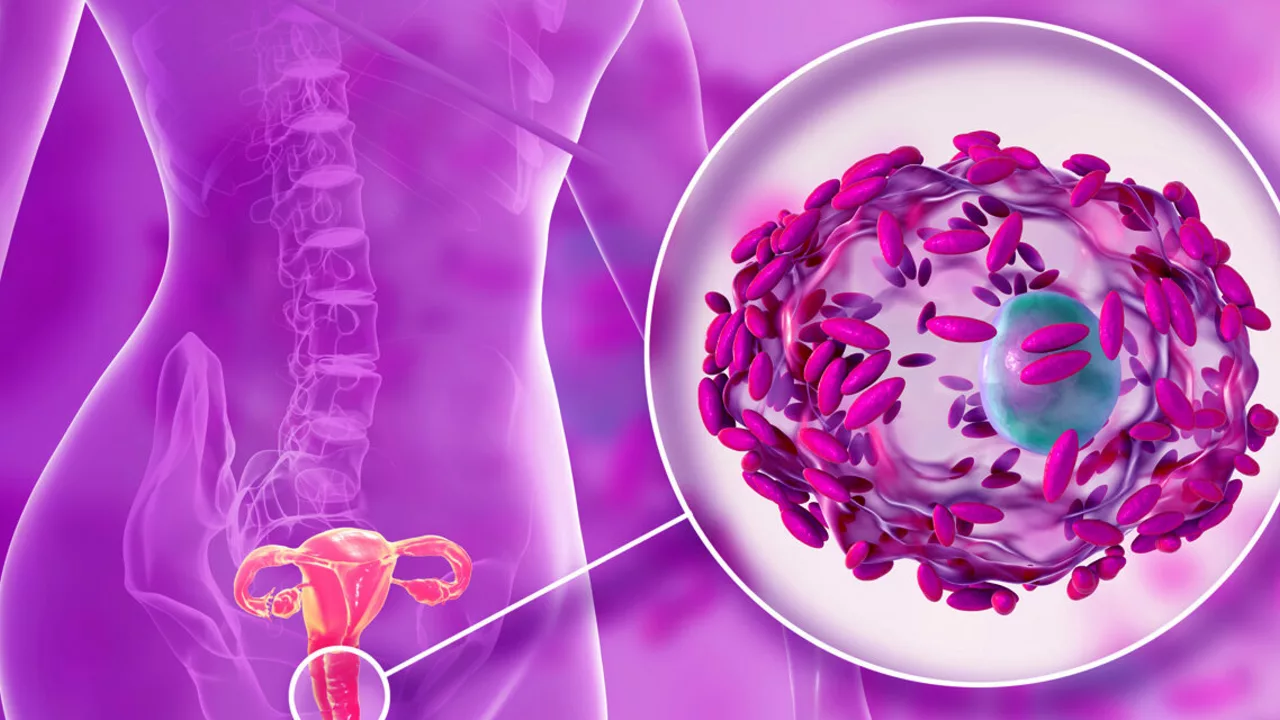
Most vaginal infections fall into three groups: yeast infection, bacterial vaginosis (BV), and trichomonas. Yeast often brings thick, white, cottage-cheese discharge with itching. BV usually causes a thin, grayish discharge and a fishy smell, especially after sex. Trichomonas (a sexually transmitted parasite) can cause greenish-yellow frothy discharge, irritation, and pain during sex or urination. Pain, fever, or heavy bleeding aren’t typical and need fast medical attention.
Simple checks you can do at home: note the color, smell, and texture of discharge, whether itching or burning is present, and if symptoms started after antibiotics, a new partner, or a new soap or product. These clues narrow the likely cause but don’t replace a test.
What to do now
If you suspect a yeast infection, short-course OTC antifungal creams or a single-dose oral pill often help. Follow the product instructions and avoid mixing treatments at once. For symptoms pointing to BV or trichomonas, don’t use OTC antifungals—those won’t work and can delay proper care. BV and trichomonas usually need prescription antibiotics like metronidazole or tinidazole, so see a clinician or sexual health clinic.
Practical at-home steps while you wait for care: stop douching, switch to unscented soap, wear breathable cotton underwear, and avoid tight synthetic fabrics. Avoid sex until symptoms clear or until your partner is treated if the infection is sexually transmitted. If symptoms are mild and this is a repeat pattern you’ve had diagnosed before, following your doctor’s prior advice can be reasonable. But if it’s your first time, symptoms are severe, or you’re pregnant, get tested.
Testing is quick: a pelvic exam and a swab can identify yeast, BV, or trichomonas. Your provider may check vaginal pH and look under a microscope. Treatment is usually straightforward, but recurrent infections need a follow-up plan—sometimes a longer course of meds or checking for underlying causes like diabetes or repeated antibiotic use.
Prevention tips that actually help: avoid unnecessary antibiotics, use condoms with new partners, dry the area after swimming or workouts, and consider a plain probiotic if you get frequent yeast infections (talk to your clinician first). If you want deeper reading on treatment options, our piece "Exploring Natural Alternatives to Flagyl" looks at options related to BV care and when they’re realistic to consider.
If you’re unsure, call your clinic. Quick testing and the right treatment stop symptoms faster and cut the chance of complications. You don’t have to guess—get the right care and get back to feeling normal.
Vaginal infections and the use of antibiotics: What you need to know
In my latest blog, I delve into the common issue of vaginal infections and the role of antibiotics in treatment. I discuss the different types of infections, such as bacterial vaginosis and yeast infections, and how they can be effectively treated with antibiotics. I also touch on the importance of proper usage of these medicines and the potential risk of antibiotic resistance. I emphasize the need for a professional diagnosis before starting any treatment, as self-diagnosing can lead to more harm than good. Lastly, I stress the importance of maintaining good vaginal health to prevent these infections.