Evidence-Based Complementary Treatments for Medication Side Effects

Side Effect Treatment Finder
Find evidence-based complementary treatments for your medication side effects while learning about potential interactions.
Evidence-Based Options
Select a side effect to see evidence-based complementary treatments.
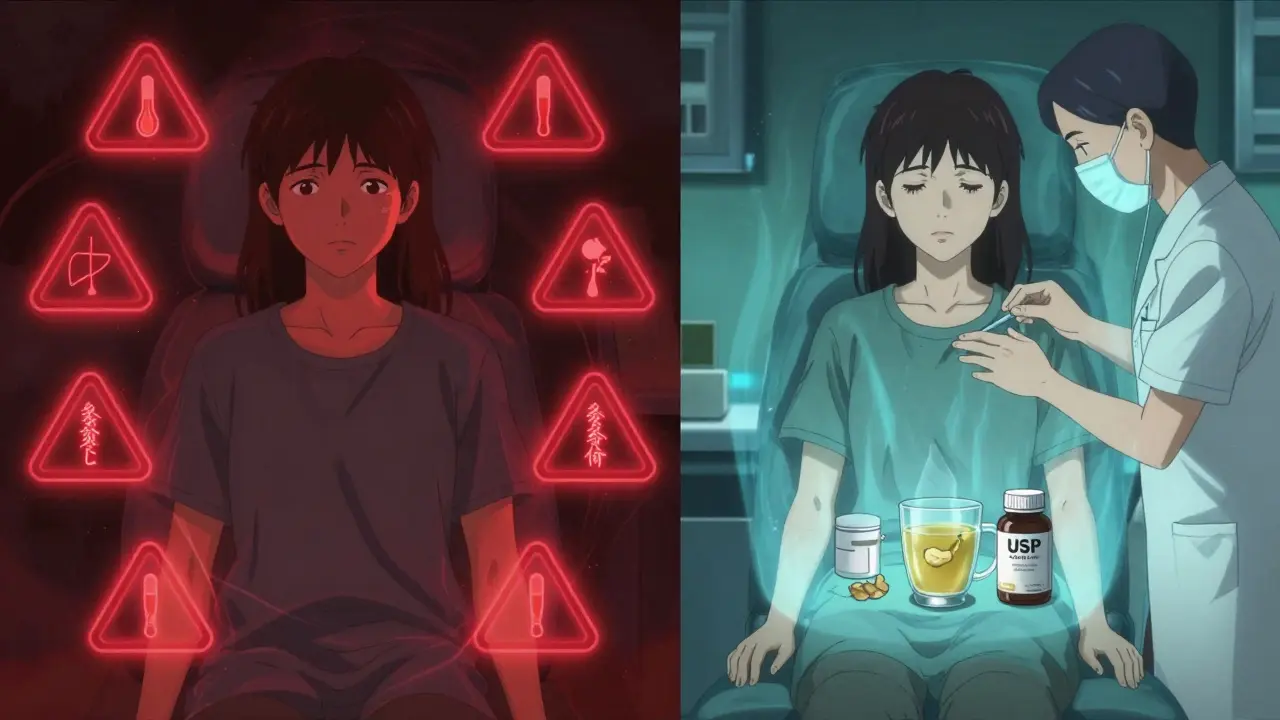
Many people take prescription medications for chronic conditions-high blood pressure, depression, cancer, diabetes-and often deal with side effects that make daily life harder. Nausea, fatigue, dry mouth, nerve pain, constipation, or dizziness aren’t just annoying; they can make people stop taking their meds altogether. That’s where complementary treatments come in-not as replacements, but as real, research-backed helpers that work alongside conventional medicine to ease the burden.
What Counts as a Complementary Treatment?
Complementary treatments are practices or products used with, not instead of, standard medical care. They’re not fringe or mystical. Many have been studied in clinical trials and shown to reduce specific side effects. The big categories include:- Natural products: Herbs, vitamins, minerals, probiotics
- Mind-body practices: Acupuncture, meditation, yoga, tai chi
- Body-based methods: Massage, chiropractic care
The most common reason people use them? To manage side effects from medications. A 2013 UK hospital study found that 45.8% of patients using complementary approaches did so specifically for this reason. And it’s not just a few people-nearly 4 in 10 U.S. adults use some form of complementary therapy, according to the National Center for Complementary and Integrative Health (NCCIH).
Acupuncture: Proven for Nausea, Constipation, and Pain
If you’ve ever felt sick after chemo or struggled with opioid-induced constipation, acupuncture might be one of the most reliable tools you haven’t tried. A 2017 meta-analysis published in JAMA Oncology looked at 20 studies involving over 2,000 cancer patients. Those who received acupuncture had a 36% greater reduction in chemotherapy-induced nausea compared to those who got sham treatments or no extra care.It’s not just nausea. A 2020 Cochrane review of 41 trials with nearly 5,000 patients found acupuncture reduced opioid-related constipation by 32% more than standard care alone. That’s significant-constipation from pain meds can be brutal, and laxatives don’t always help.
For nerve pain from chemotherapy (called peripheral neuropathy), patients report real relief. One verified patient on Trustpilot said acupuncture cut their taxol-induced nerve pain by half. And unlike pills, acupuncture doesn’t add more chemicals to your system. It’s low-risk when done by a licensed practitioner using sterile needles.
Ginger: A Kitchen Staple That Actually Works
You don’t need a clinic visit to try ginger. It’s in your spice rack. And science backs it up. Multiple studies show that taking 0.5 to 1.0 gram of ginger daily-whether as capsules, tea, or chewable pieces-can reduce chemotherapy-induced nausea by up to 40%.A 2013 study in the Journal of Pain and Symptom Management compared ginger to a placebo in cancer patients. Those who took ginger reported significantly less vomiting and less need for anti-nausea drugs. One Reddit user, u/ChemoSurvivor2022, shared: “Ginger capsules reduced my nausea by 70% compared to ondansetron alone.”
It’s not just for cancer. Ginger has also been shown to help with motion sickness and post-op nausea. The dose is simple: 250-500 mg, taken 3-4 times a day. It’s affordable, accessible, and safe for most people. But if you’re on blood thinners like warfarin, talk to your doctor first-ginger can mildly affect clotting.
Herbs: Powerful, But Use With Caution
Herbs aren’t harmless. Just because they’re “natural” doesn’t mean they’re safe with your meds. Some have serious interactions.Hawthorn, often used for heart health, is generally well tolerated and may help with mild high blood pressure. But the American Heart Association warns it could theoretically interact with ACE inhibitors or beta-blockers. While studies show it doesn’t cause major problems when used together, the risk isn’t zero.
Garlic supplements are popular for cholesterol, but they can boost the effect of blood thinners like aspirin or lisinopril. One UK hospital study flagged 82 patients out of 179 for potential garlic-drug interactions. That’s nearly half.
And then there’s the scary stuff. Milk thistle is often taken to “protect the liver” during chemo. But one Reddit user, u/CancerWarrior87, ended up hospitalized after taking it-liver toxicity. Blue cohosh can spike blood pressure and heart rate. Lily of the valley is dangerously toxic if taken with digoxin, a common heart drug, because it can drop potassium to life-threatening levels.
Bottom line: If you’re thinking about herbs, don’t guess. Use the About Herbs app from Memorial Sloan Kettering (updated September 2023) or the NCCIH’s online interaction checker. Both are free and updated monthly.
Supplements: The Wild West of the Market
The supplement industry is barely regulated. In the U.S., the Dietary Supplement Health and Education Act of 1994 lets companies sell products without proving safety or effectiveness. That means:- What’s on the label might not be in the bottle
- Contaminants like heavy metals or hidden pharmaceuticals are common
- Doses can be way higher than recommended
A 2018 study of 318 cancer patients found 11% were taking supplements at doses above the recommended amount. One patient took 1,000 mg of vitamin C daily-far above the safe upper limit-thinking it would help. Instead, it interfered with their chemo.
Antioxidants like vitamins A, C, E, and selenium are especially tricky. Cancer Research UK warns they might protect cancer cells from being damaged by radiation or chemo. The evidence isn’t conclusive, but the risk is real enough that many oncologists advise patients to avoid high-dose antioxidants during treatment.
Why Disclosure Matters More Than You Think
Here’s the biggest problem: most people don’t tell their doctors.In the same UK hospital study, only 20.9% of patients using complementary treatments disclosed them to their healthcare team. That’s alarming. If you’re taking ginger, turmeric, or a “natural” sleep aid, your doctor doesn’t know. And they can’t warn you about interactions.
Imagine you’re on blood pressure meds, and you start taking hawthorn extract. Your doctor adjusts your dose based on what they think you’re taking. But if you’re also using garlic pills and fish oil, your blood pressure could crash. That’s not hypothetical-it’s documented.
Doctors aren’t always trained in herbal interactions. A 2021 study found most physicians need at least 20 hours of training to confidently assess CAM risks. That’s why it’s on you to speak up.

How to Use Complementary Treatments Safely
You don’t need to avoid these options. You just need to use them wisely. Here’s how:- Don’t stop your meds. Never discontinue or change your prescription without talking to your doctor.
- Disclose everything. Tell your doctor and pharmacist every supplement, herb, or therapy you use-even if you think it’s “just ginger.”
- Start low, go slow. Try one new thing at a time. Give it 2-4 weeks to see if it helps.
- Choose quality. Look for products with third-party testing seals: USP, NSF, or ConsumerLab.
- Track your symptoms. Keep a simple log: what you took, when, and how you felt. It helps your doctor spot patterns.
For cancer patients, integrative oncology programs are now available in 73% of U.S. cancer centers. These teams include doctors trained in both conventional and complementary care. They don’t push herbs-they evaluate them. If you’re undergoing treatment, ask if your hospital offers this service.
What’s New in 2026?
Research is moving fast. In 2023, the NIH launched the Precision CAM initiative to find biomarkers that predict who will respond to which complementary therapy. The goal? Personalized care-knowing before you start whether ginger or acupuncture will work for you, not just someone else.The FDA issued a warning in April 2023 about kratom products linked to 195 deaths since 2016. That’s a reminder: unregulated doesn’t mean safe. Stick to well-studied options with clear safety profiles.
The global market for complementary therapies is growing at 11.4% a year. But the real win isn’t sales-it’s better quality of life. Patients who use evidence-based complementary treatments report less pain, less nausea, and more control over their health.
Final Thought: It’s About Partnership, Not Replacement
Complementary treatments aren’t magic. They’re tools. And like any tool, they work best when used with knowledge and care. The goal isn’t to swap pills for herbs. It’s to reduce suffering without adding new risks.If you’re struggling with side effects, talk to your doctor. Ask: “Are there any evidence-based complementary options that might help with this?” Then bring your list of what you’re already using. That’s how you turn confusion into control.
Can complementary treatments replace my medication?
No. Complementary treatments are meant to work alongside your prescribed medications-not replace them. Stopping your meds can lead to serious health risks. Always talk to your doctor before making any changes.
Is acupuncture safe if I’m on blood thinners?
Yes, when performed by a licensed practitioner using sterile, single-use needles. There’s no evidence that acupuncture increases bleeding risk in people on blood thinners like warfarin or aspirin. But always inform your acupuncturist about your medications.
Which herbs are most likely to interact with my drugs?
Garlic, ginkgo, ginger, ginseng, St. John’s wort, and echinacea are among the most common culprits. Garlic and ginkgo can increase bleeding risk with anticoagulants. St. John’s wort can reduce the effectiveness of antidepressants, birth control, and heart meds. Always check interactions before starting any herb.
Are natural supplements regulated like prescription drugs?
No. In the U.S., supplements are regulated as food, not medicine. That means they don’t need to prove safety or effectiveness before being sold. Contamination and mislabeling are common. Look for third-party testing seals like USP or NSF to reduce risk.
Should I take antioxidants like vitamin C during chemotherapy?
Many oncologists advise against high-dose antioxidants during chemo or radiation because they might protect cancer cells from treatment. While the evidence isn’t final, the potential risk outweighs the unproven benefit. Stick to getting antioxidants from whole foods, not pills.
How do I know if a complementary treatment is evidence-based?
Look for studies published in peer-reviewed journals like JAMA, The Lancet, or Cochrane Reviews. Reliable sources include the National Center for Complementary and Integrative Health (NCCIH), Memorial Sloan Kettering’s About Herbs database, and Cancer Research UK. Avoid sites that sell products or use words like “miracle cure.”






Comments
Ted Conerly
January 10, 2026 AT 01:00Acupuncture for chemo nausea actually works better than I thought. I had a buddy on treatment who swore by it after three sessions. No more vomiting, no more hitting the anti-nausea meds hard. Just quiet, steady relief. Worth trying if your doc is open to it.
Faith Edwards
January 10, 2026 AT 01:48One mustn't confuse the venerable traditions of Eastern medicine with the haphazard, unregulated pharmacopeia of the modern wellness-industrial complex. Ginger capsules? How quaint. But to casually endorse them alongside pharmaceuticals without rigorous, double-blind, placebo-controlled longitudinal studies is to invite medical anarchy.
Jay Amparo
January 11, 2026 AT 23:49I’ve seen this in my own family in India-my aunt used turmeric paste for joint pain while on arthritis meds, and her doctor was shocked she didn’t tell them. But she didn’t think it mattered because it was ‘just spice.’ That’s the real issue here: we treat herbs like snacks, not substances with real pharmacology. Talk to your provider. Seriously.
Lisa Cozad
January 13, 2026 AT 12:37Just wanted to add that I started ginger tea during my last round of chemo and it made a noticeable difference in nausea. Not magic, but it helped. Also, I kept a little journal-what I took, when, how I felt. It made my oncologist’s job way easier. Small habits, big impact.
Saumya Roy Chaudhuri
January 15, 2026 AT 05:36Let’s be clear-acupuncture is placebo at best. The whole concept of qi is pseudoscientific nonsense. And ginger? It’s just a mild COX inhibitor. You’re better off sticking to FDA-approved antiemetics. The fact that people treat this like medicine is why American healthcare is in such a mess.
Ian Cheung
January 16, 2026 AT 21:22Been on blood pressure meds for 12 years and started taking garlic capsules because my cousin said it lowered his cholesterol. Didn’t realize it was making my BP drop too low till I passed out in the shower. Now I check every supplement with my pharmacist. Don’t be like me. Just ask.
anthony martinez
January 18, 2026 AT 08:27Oh great, another article telling us to ‘talk to our doctors’ like they’re all trained in herbal interactions. Most of them can’t even spell ‘Cochrane’ and think ‘natural’ means ‘safe.’ Meanwhile, the supplement aisle is a minefield of unlabeled caffeine and heavy metals. Good luck.
Mario Bros
January 19, 2026 AT 17:30My mom did acupuncture for nerve pain after chemo and it was a game-changer. She’s not some hippie-she’s a retired accountant. If it helped her, it’s worth a shot. Just find a licensed pro. And skip the sketchy Amazon supplements. 🙏
Jake Nunez
January 21, 2026 AT 10:36In my village in Nigeria, we use bitter leaf for hypertension. No one calls it ‘complementary’-it’s just how we’ve always done it. The science might be catching up, but the wisdom? It’s been here. We need more cross-cultural respect in these conversations, not just Western validation.
Christine Milne
January 23, 2026 AT 09:46Let me be perfectly clear: the notion that ginger, a plant native to Southeast Asia, possesses therapeutic efficacy equal to pharmaceutical-grade ondansetron is not merely scientifically dubious-it is a dangerous affront to evidence-based medicine. The proliferation of such misinformation is a direct consequence of anti-intellectualism in public discourse.
Bradford Beardall
January 24, 2026 AT 09:29I’m curious-has anyone here tried mindfulness meditation for fatigue from long-term statin use? I’ve read a few small studies, but I’d love to hear real-world experiences. Not just cancer patients-people on meds for depression, diabetes, whatever. What worked?
McCarthy Halverson
January 26, 2026 AT 03:25Disclose everything. Even the turmeric. Even the chamomile tea. Even the CBD gummies you think no one notices. Your doctor can’t help if they don’t know. Simple.
Michael Marchio
January 27, 2026 AT 19:00Look, I get it. You’re tired. You’re in pain. You want something that feels like it’s working without the side effects of more pills. But let’s be honest here-most people who turn to ‘complementary’ treatments are desperate, not informed. And desperation makes you vulnerable. The supplement industry knows this. They prey on it. They sell you hope wrapped in pretty packaging and a ‘100% natural’ label. Meanwhile, the real science? It’s buried under five layers of marketing and influencer testimonials. Don’t be the person who reads one Reddit thread and decides to swap their beta-blocker for hawthorn. That’s not empowerment. That’s a one-way ticket to the ER.