Hormone Replacement Therapy: What You Need to Know About Benefits, Risks, and Monitoring
For millions of women going through menopause, the sudden wave of hot flashes, night sweats, sleepless nights, and brain fog isn’t just annoying-it’s exhausting. Many feel like their body has betrayed them. Hormone Replacement Therapy (HRT) has been around since the 1940s, but its reputation has swung wildly-from miracle cure to dangerous gamble-and back again. Today, the truth is more balanced, more personal, and more nuanced than the headlines suggest.
What HRT Actually Does
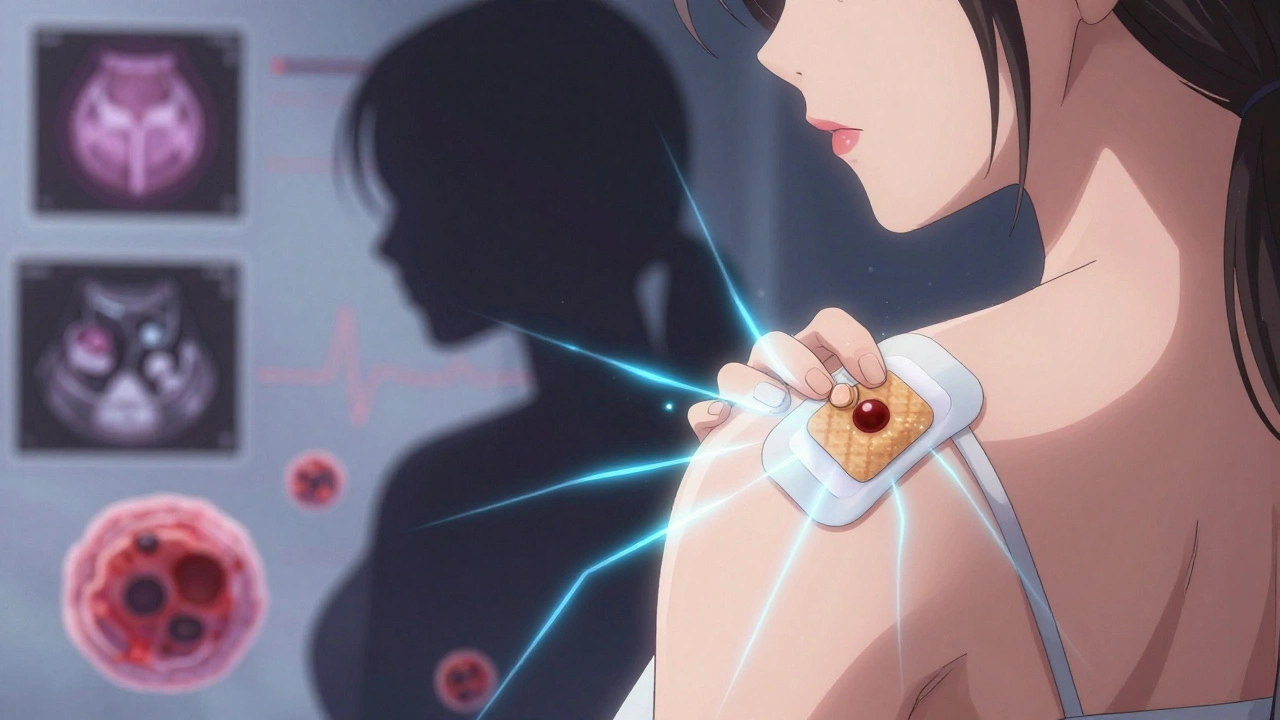
HRT replaces the estrogen (and sometimes progesterone) your body stops making after menopause. It’s not a one-size-fits-all pill. There are different types: estrogen-only for women who’ve had a hysterectomy, and estrogen plus progestogen for those with a uterus (to protect the lining of the womb). You can take it as a pill, a patch, a gel, a vaginal ring, or even an implant.
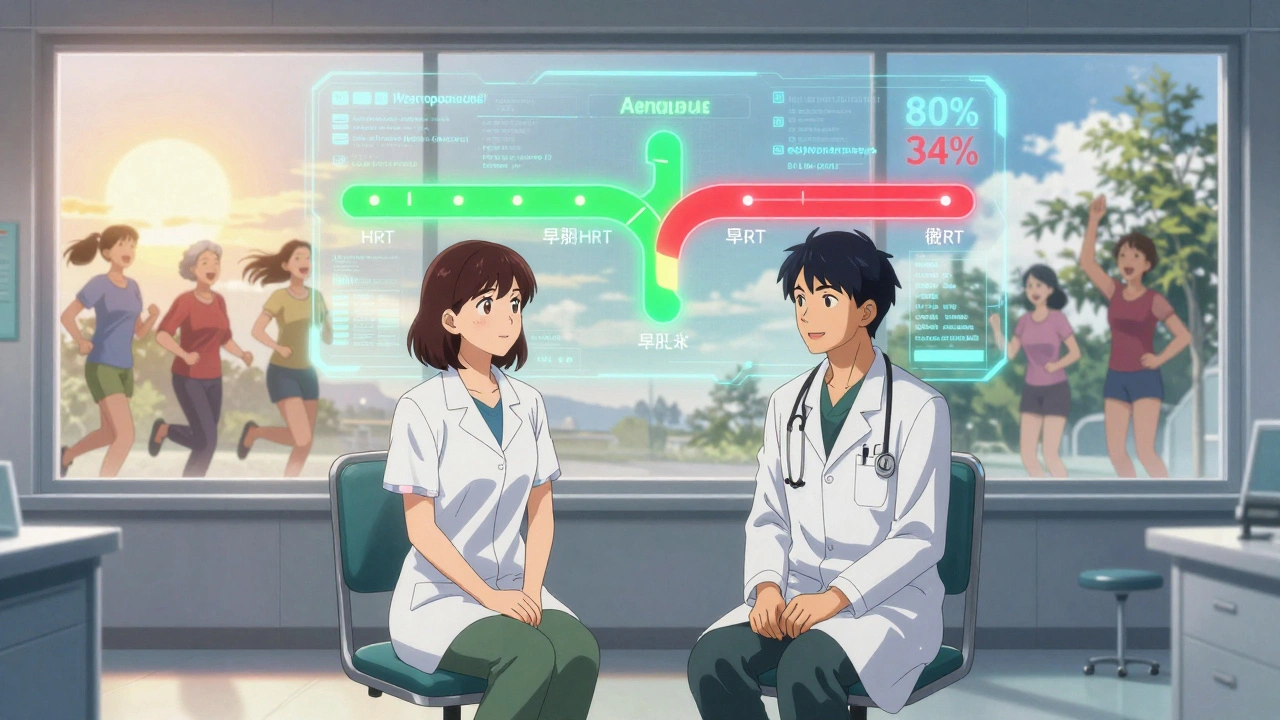
The most effective use of HRT is for managing moderate to severe menopausal symptoms. If you’re having hot flashes that wake you up three times a night or vaginal dryness that makes sex painful, HRT works better than anything else. Studies show it reduces hot flashes by 80-90%, compared to about 50-60% for antidepressants like SSRIs. That’s a massive difference in daily quality of life.
It also protects your bones. Women on HRT have a 34% lower risk of fractures from osteoporosis than those who don’t. That’s not just about avoiding a broken hip-it’s about staying independent as you age.
The Risks: What the Data Really Says
The big scare came in 2002 with the Women’s Health Initiative (WHI) study. It found a small but real increase in breast cancer, blood clots, and stroke among women taking HRT. That led to a 70% drop in prescriptions overnight. But here’s what got lost in the noise: the study mostly included women over 60, many of whom had been postmenopausal for more than 10 years. That’s not who HRT is meant for.
Current guidelines, updated by the FDA in September 2022, make this clear: HRT is safest and most beneficial when started before age 60 or within 10 years of your last period. For women in that window, the benefits outweigh the risks.
Let’s break down the real numbers:
- Breast cancer risk: For women taking estrogen plus progestogen, there are about 8 extra cases per 10,000 women per year. That’s a small increase, especially compared to other risk factors like obesity or alcohol use. Estrogen-only therapy doesn’t increase breast cancer risk at all.
- Blood clots: Oral HRT raises the risk of deep vein thrombosis (DVT) to about 3.7 per 1,000 women per year. Transdermal (patch or gel) cuts that risk in half-down to 1.3 per 1,000. That’s why many doctors now start with patches or gels.
- Stroke: Oral estrogen slightly increases stroke risk, especially in older women. Transdermal estrogen shows no increased risk in most studies.
- Heart disease: When started early, HRT actually lowers heart disease risk by 32%. Started late? No benefit. That’s why timing matters more than the drug itself.
And here’s something surprising: some recent data suggests HRT might reduce overall mortality in younger menopausal women. The Endocrine Society and the North American Menopause Society both now say that for healthy women under 60, HRT isn’t just safe-it can be life-enhancing.
Bioidentical vs. Synthetic: What’s the Difference?
You’ve probably heard of “bioidentical hormones.” These are marketed as “natural” and “safer,” often sold as custom-compounded creams or pellets. But here’s the catch: the FDA and the Endocrine Society say there’s no proof they’re safer than FDA-approved versions. Compounded products aren’t tested for consistency, purity, or long-term safety. One batch might have too much estrogen. Another might have none.
Approved HRT products-like estradiol patches, micronized progesterone pills, or conjugated estrogens-are manufactured to precise standards. They come with clear dosing, known side effects, and decades of research behind them. If you want “natural,” choose FDA-approved bioidentical estradiol and progesterone. Skip the compounding pharmacies unless you’re in a clinical trial.
How HRT Is Monitored: What Your Doctor Should Do
HRT isn’t a set-it-and-forget-it treatment. It needs regular check-ins. Before starting, your doctor should:
- Check your blood pressure
- Do a breast exam
- Order a mammogram
- Review your personal and family history of cancer, blood clots, or heart disease
- Measure your BMI (weight matters-obesity increases HRT risks)
After you start:
- First follow-up at 3 months: Are symptoms improving? Any new side effects like bloating, breast tenderness, or headaches?
- Annual check-ups: Blood pressure, weight, breast exam, and discussion about whether you still need HRT.
- Mammogram every 1-2 years, depending on your risk.
One of the most common concerns is irregular bleeding in the first 6 months. That’s normal when you’re on a combination regimen. But if bleeding continues past 6 months, you need an endometrial biopsy to rule out abnormal cell growth. That’s not a scare tactic-it’s standard care.
Who Should Avoid HRT
HRT isn’t for everyone. You should not start it if you have:
- A history of breast cancer
- Active blood clots or a history of deep vein thrombosis or pulmonary embolism
- Unexplained vaginal bleeding
- Severe liver disease
- History of stroke or heart attack
Even if you’re under 60, if you have a strong family history of breast cancer or clotting disorders, talk to a specialist. Genetic testing for BRCA mutations or thrombophilia might help guide your decision.
Real Stories, Real Outcomes
Women who stick with HRT often say it changed their lives. A 2020 study found 78% of women on HRT reported major improvement in hot flashes within 3 months. Cleveland Clinic surveys show transdermal users are more likely to stay on treatment-68% after a year, compared to just 52% for pill users. Why? Fewer side effects. Less nausea. Fewer mood swings.
But many quit because they’re scared. In one survey, 48% of women who stopped HRT said they feared breast cancer-even though their personal risk was low. That fear often comes from outdated information. The FDA removed its blanket black box warning in 2022 because it was misleading. HRT isn’t a gamble-it’s a tool. And like any tool, it works best in the right hands, at the right time.
What’s Next for HRT
Research is moving fast. Scientists are now looking at how your genes affect how you process estrogen. Variants in the CYP1B1 gene can predict how your body metabolizes estradiol-with 62% accuracy. That could one day mean personalized dosing based on your DNA.
New formulations are also coming. TSECs (tissue-selective estrogen complexes), like Duavee, combine estrogen with a drug that protects the breast and uterus. They’ve shown promise in reducing endometrial thickening without needing a separate progesterone pill.
And transdermal progesterone? Still in development. Right now, oral progesterone can cause drowsiness and mood changes. A patch or gel version could be a game-changer.
For now, the best advice is simple: if you’re under 60 and struggling with menopause symptoms, HRT is still the most effective option. Don’t let old fears stop you. Talk to your doctor. Ask about transdermal options. Start low. Monitor closely. And don’t assume HRT is all risk-because for most women, the real risk is not treating the symptoms at all.
Is HRT safe for women over 60?
For women over 60 or more than 10 years past menopause, HRT is generally not recommended for long-term use. The risks of blood clots, stroke, and possibly breast cancer increase with age and time since menopause. If you’re over 60 and still having severe symptoms, talk to your doctor about low-dose, short-term options-but only after evaluating your heart and breast health. Non-hormonal treatments may be safer for you.
Do I need progesterone with HRT?
Yes-if you still have your uterus. Estrogen alone can cause the lining of the uterus to thicken, which raises the risk of endometrial cancer. Progesterone (or progestogen) balances that out. Micronized progesterone (like Prometrium) is preferred over synthetic versions because it’s better tolerated and linked to lower breast cancer risk. If you’ve had a hysterectomy, you don’t need it.
Can HRT cause weight gain?
HRT itself doesn’t cause weight gain. Weight gain during menopause is usually due to aging, reduced muscle mass, and changes in metabolism. Some women report bloating or water retention early on, especially with oral estrogen. Switching to a transdermal patch or gel often helps. The key is staying active and eating well-HRT won’t fix poor lifestyle habits, but it can make it easier to stick with them by improving sleep and energy.
How long should I stay on HRT?
There’s no fixed timeline. Most women take HRT for 2-5 years to get through the worst symptoms. But some need it longer-especially if they have early menopause or severe bone loss. The goal is to use the lowest dose that works and reassess every year. If your symptoms fade, you can try tapering off. If they come back, restarting at a low dose is often safe if you’re still under 60.
What are the alternatives to HRT?
For hot flashes, options include SSRIs like paroxetine (Brisdelle), gabapentin, or clonidine-but they’re less effective than HRT. Lifestyle changes help too: cooling your bedroom, avoiding caffeine and alcohol, practicing paced breathing. For vaginal dryness, non-hormonal lubricants or low-dose vaginal estrogen (which doesn’t enter the bloodstream) are safe and effective. For bone health, calcium, vitamin D, weight-bearing exercise, and medications like bisphosphonates are alternatives, but they don’t touch hot flashes.
Is HRT right for me if I have a family history of breast cancer?
It depends. If you have a BRCA mutation or a strong family history, estrogen-only HRT may still be an option if you’ve had a hysterectomy. Estrogen plus progesterone carries more risk. Talk to a breast specialist or menopause expert. Genetic testing and risk models like Gail or Tyrer-Cuzick can help. Some women choose to avoid HRT entirely and rely on non-hormonal treatments. Others take HRT for a short time and monitor closely with extra screenings. There’s no single answer-personalized care is key.






Comments
Anthony Breakspear
December 3, 2025 AT 07:49Honestly? I wish I’d known this stuff 5 years ago. My mom went through menopause like a dragon with a fever, and no one told her HRT could’ve made her life bearable. She suffered in silence because of fear-mongering headlines. Now she’s on a patch, sleeps through the night, and actually laughs again. Stop letting fear decide your health.
Zoe Bray
December 3, 2025 AT 09:20While the article presents a compelling synthesis of current clinical guidelines, it is imperative to underscore the distinction between relative risk and absolute risk in the context of hormone replacement therapy. The Women’s Health Initiative cohort was not representative of the target demographic for early initiation, and subsequent meta-analyses (e.g., Manson et al., 2017) confirm a favorable benefit-risk ratio when initiated within the therapeutic window. Furthermore, transdermal estrogen bypasses first-pass hepatic metabolism, thereby mitigating thrombotic risk-critical for clinical decision-making.
Sheryl Lynn
December 4, 2025 AT 15:18Oh honey, let’s not pretend this is science-it’s just Big Pharma repackaging estrogen as ‘empowerment’ while the compounding pharmacies quietly laugh all the way to the bank. Bioidentical? Please. If it’s not FDA-approved and stamped with a barcode, it’s basically witchcraft with a prescription pad. And don’t get me started on the ‘natural’ crowd who think soy is a hormone and yoga cures osteoporosis.
Paul Santos
December 6, 2025 AT 03:19Interesting how we’ve turned menopause into a medical crisis instead of a natural transition. 🤔 The real issue? We’ve infantilized women’s bodies and then monetized their fear. HRT isn’t the answer-it’s the symptom of a culture that can’t tolerate aging. Also, patches > pills. Always. 🧪
Eddy Kimani
December 6, 2025 AT 22:25One thing the article doesn’t dive into: the role of SHBG (sex hormone-binding globulin) in modulating free estrogen levels. Variability here can explain why two women on identical doses have wildly different symptom responses. Also, CYP1A2 and CYP3A4 polymorphisms affect estrogen metabolism-could be huge for personalized dosing down the line. Anyone else tracking this?
Chelsea Moore
December 8, 2025 AT 17:55STOP. RIGHT. NOW. This is just another way to poison women under the guise of ‘helping.’ Did you know estrogen is linked to breast cancer? Did you know it’s a carcinogen? The FDA changed their warning because they’re bought off by drug companies! My aunt died from a blood clot after HRT-don’t you dare tell me it’s ‘safe’! You’re all just scared of aging, and now you want to chemically fix it?! I’m not having this!
John Biesecker
December 10, 2025 AT 17:10man i had no idea patches were so much safer than pills 😅 i switched last year after my doc mentioned it and wow-no more nausea, i sleep like a baby, and my mood stopped being a rollercoaster. also, i didn’t know bioidentical was just a fancy word for untested stuff… yikes. thanks for the clarity 🙏
Genesis Rubi
December 12, 2025 AT 15:39Why are we letting doctors in the US decide what women do with their bodies? In China they use herbs and acupuncture and women live to 100 without hormones. This is just western medicine trying to control us. Also, estrogen is for weak people. I’m 58 and I’ve never taken a pill. I’m stronger than all of you.
Doug Hawk
December 13, 2025 AT 20:49Just wanted to say the part about irregular bleeding being normal in the first 6 months saved me. I was terrified I had cancer. My doc said it was expected and we just watched it. No biopsy needed. Also, the point about BMI being a factor? Huge. I lost 20 lbs and my hot flashes cut in half. HRT helped but lifestyle mattered too. Thanks for the real talk.
John Morrow
December 14, 2025 AT 17:12While the article superficially addresses risk-benefit ratios, it fails to interrogate the underlying epistemological framework that privileges pharmaceutical intervention over physiological adaptation. The assumption that menopause is a deficit to be corrected rather than a transition to be integrated reflects a pathological medicalization of aging-a phenomenon deeply rooted in capitalist healthcare structures that profit from perpetual pharmacological dependency. The data may be statistically sound, but the narrative remains unchallenged: women’s bodies are broken until fixed by industry-approved chemicals.
Kristen Yates
December 16, 2025 AT 08:42I’m from Kenya. In my village, women go through menopause and keep working. They drink bitter leaf tea, wear loose clothes, and talk to each other. No pills. No patches. No panic. Maybe we don’t need to fix what isn’t broken.
Saurabh Tiwari
December 17, 2025 AT 10:09cool article bro. i live in india and we have a lot of women on hrt now. my mom is on it and she feels way better. but i also know women who use ayurvedic stuff like shatavari and it works too. maybe both can coexist? just saying
Michael Campbell
December 18, 2025 AT 07:03they’re lying. it’s all about control. the government, the pharma, the doctors-they want you dependent. you think you’re getting relief? you’re getting addicted. they don’t care if you live or die as long as you keep buying.
Victoria Graci
December 18, 2025 AT 23:17I love how this article doesn’t just say ‘take HRT’-it says ‘talk to your doctor.’ That’s the real win. Medicine isn’t about one-size-fits-all. It’s about listening. My grandma took HRT for 15 years. My aunt refused it. Both are fine. The difference? One had a doctor who asked her how she felt, not just what her labs said. That’s the magic. Not the pill. The conversation.