How to Calculate Total Cost of Therapy Beyond the Copay
Most people think they know how much therapy will cost because they see a copay on their insurance card-maybe $30 or $50 per session. But that number is just the tip of the iceberg. The real cost of therapy includes your deductible, coinsurance, session frequency, whether your therapist is in-network, and even your monthly premium. If you don’t factor all this in, you could end up shocked when you get your first bill.
What You’re Really Paying: More Than Just the Copay
Your copay is the fixed amount you pay at each session, but it only kicks in after you’ve met your deductible. If you haven’t met your deductible yet, you pay the full session rate-no matter what your card says. For example, if your therapist charges $125 per session and your deductible is $1,500, you’ll pay $125 for each session until you’ve spent $1,500 out of pocket. That’s 12 sessions before your copay even applies.Thriveworks’ 2024 study found that the average uninsured therapy session costs $143.26. With insurance, you might think you’re getting a deal, but if you’re still in your deductible phase, you’re paying close to that full price. And if you need 16 sessions to feel better, as many patients do, you could be paying over $2,000 before insurance starts covering part of it.
Deductibles: The Hidden Upfront Cost
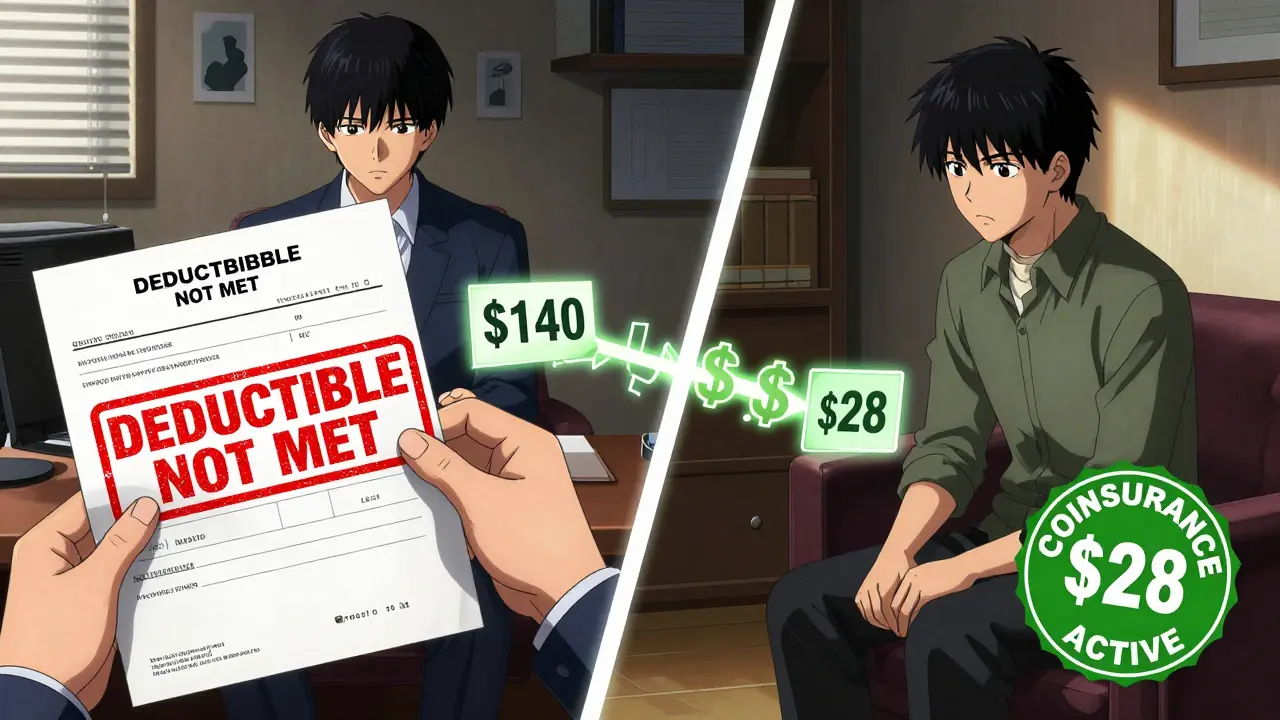
A deductible is the amount you pay each year before your insurance starts sharing the cost. For mental health services, this can be separate from your medical deductible. Some plans have a mental health-specific deductible, which means even if you’ve paid your $1,500 medical deductible through doctor visits or lab tests, you still have to pay another $1,500 for therapy.Let’s say you have a $3,000 deductible for mental health. If each session is $140, you’ll pay the full $140 for each session until you’ve spent $3,000. That’s about 21 sessions before your insurance starts helping. If you’re seeing your therapist weekly, you’ll hit that deductible in under five months. And if you need 20-25 sessions to recover from anxiety or PTSD, as Grow Therapy found, you’re already in deep.
Coinsurance: When You Pay a Percentage
Once you meet your deductible, coinsurance kicks in. This is the percentage you pay after that. Most plans use 20% or 30%. So if your therapist charges $140 per session and your coinsurance is 20%, you pay $28 per session. Sounds good, right? Not if your total therapy costs add up to $30,000.Here’s the math: You pay your $3,000 deductible first. Then, for the remaining $27,000 in therapy costs, you pay 20%-that’s $5,400. Your total out-of-pocket? $8,400. Even with insurance, you’re still paying more than most people expect. And this isn’t rare. A 2023 analysis from Alma showed that patients with high-deductible plans and long-term therapy needs often pay more than $6,000 annually just for mental health services.
In-Network vs. Out-of-Network: A Huge Difference
Choosing an in-network therapist can cut your costs by half. In-network providers have agreed to accept the insurance company’s “allowed amount” as full payment. For example, if your therapist normally charges $180 but the insurance allows only $120, you’ll pay based on $120-not $180.Out-of-network therapists don’t have that agreement. You pay the full fee upfront, then submit a claim. Your insurance might reimburse you 50%-70% of the allowed amount, but you’re still on the hook for the rest. Some patients end up paying $100-$150 per session out-of-pocket, even with insurance, because their plan doesn’t cover out-of-network care well.
And location matters. In New York, therapy averages $176 per session. In North Dakota, it’s $227. So if you’re paying 30% coinsurance, you’re paying $53 in New York-but $68 in North Dakota. Same plan. Different city. Big difference in your wallet.
What About Medicare and Medicaid?
If you’re on Medicare, you pay 20% of the approved amount after meeting your Part B deductible. That usually comes out to about $28.65 per session. But if you have Original Medicare, you’ll need a Medigap Plan G to cover that 20%. Those plans cost $100-$200 per month, so your total monthly cost could be $128.65 if you’re seeing your therapist weekly.Medicaid, on the other hand, often has little to no copay. In many states, therapy is fully covered. But eligibility and coverage vary widely. If you’re on Medicaid, check your state’s mental health benefits before assuming anything.
How Many Sessions Do You Really Need?
Most people assume therapy lasts 6-8 weeks. But that’s not the norm. Thriveworks’ 2024 data shows that 50% of patients need 15-20 sessions to see meaningful improvement. For complex conditions like trauma, depression, or OCD, 30+ sessions are common. If you’re paying $40 per session after your deductible, and you need 20 sessions, that’s $800. But if you’re still paying full price because you haven’t met your deductible? That’s $2,500 before insurance helps.Shasta Health found that nearly 40% of patients didn’t know their true out-of-pocket cost until after they’d already started therapy. That’s because they only looked at the copay-not the deductible, coinsurance, or session frequency.
Sliding Scale and Alternative Options
If you’re uninsured or underinsured, you’re not stuck. About 42% of private practice therapists offer sliding scale fees based on income. That can cut your cost by 30-50%. For example, if you’d normally pay $140 per session, you might pay $70-$98 instead.Platforms like Open Path Collective offer therapy for $40-$70 per session to people without insurance. University training clinics-where graduate students provide therapy under supervision-often charge 50-70% less than private practices. These aren’t second-rate options. Many clients report the same outcomes as with private therapists.
Building Your Real Therapy Budget
Here’s how to calculate your total cost step by step:- Find your insurance plan type: Is it copay, deductible, or coinsurance-based?
- Check if mental health has a separate deductible.
- Know your in-network vs. out-of-network rates.
- Estimate how many sessions you’ll need (12-20 is typical).
- Calculate Phase 1: Full price until deductible is met.
- Calculate Phase 2: Copay or coinsurance after deductible.
- Check your out-of-pocket maximum ($9,350 for individuals in 2024).
- Add monthly premiums (multiply by 12).
- Factor in medication costs if you’re taking any.
Example: You have a $1,500 deductible, 20% coinsurance, and see a therapist who charges $125/session. You need 20 sessions.
- Phase 1: Pay $125 x 12 sessions = $1,500 (deductible met)
- Phase 2: Pay 20% of $125 = $25 per session x 8 sessions = $200
- Total: $1,700
Without insurance? $2,500. With insurance? $1,700. That’s a 32% savings-but only if you understand the full picture.
Tools to Help You Track Costs
- Use your insurance company’s online portal to check your deductible status and allowed amounts.Don’t wait until you’re in crisis to figure this out. Start early. Call your insurer. Ask for a breakdown of your mental health benefits. Write it down. Track your spending. You’ll thank yourself later.
Is the copay the only thing I pay for therapy?
No. The copay is only what you pay after meeting your deductible. Before that, you pay the full session rate. You may also pay coinsurance (a percentage of the cost), monthly premiums, and out-of-network fees. The copay is just one piece of the puzzle.
What if I haven’t met my deductible yet?
You’ll pay the full price of each therapy session until you’ve spent your deductible amount. For example, if your deductible is $1,500 and each session costs $125, you’ll pay $125 for each of the first 12 sessions. Only after that will your copay or coinsurance apply.
Can I use other medical expenses to meet my mental health deductible?
Yes-if your plan uses a combined deductible. Many plans count all covered medical services (doctor visits, lab tests, prescriptions) toward the same deductible. So if you’ve already spent $1,000 on physical therapy or prescriptions, that counts toward your mental health deductible. Check your plan details to confirm.
Does Medicare cover therapy differently?
Yes. Medicare Part B covers 80% of therapy costs after you meet the Part B deductible. You pay 20%-about $28.65 per $143 session. But if you have Original Medicare, you’ll need a Medigap Plan G to cover that 20%. Plan G has its own monthly premium, so your total cost includes both.
How do I know if my therapist is in-network?
Call your insurance provider and ask for a list of in-network mental health providers. You can also check their website or use tools like Alma or Zocdoc, which show network status. Never assume-some therapists list themselves as in-network but aren’t actually contracted with your plan.
Are there affordable options if I can’t afford therapy?
Yes. About 42% of private therapists offer sliding scale fees based on income. Open Path Collective offers sessions for $40-$70. University training clinics often charge 50-70% less than market rates. Community health centers and online platforms like BetterHelp also have financial aid programs. Don’t give up-affordable help exists.




