Menopause and Sleep: Practical Tips for Better Rest

When the nighttime routine starts to feel like a battle, you’re not alone. Many women going through Menopause a natural stage marked by the end of menstrual cycles, typically occurring between ages 45 and 55 discover that a good night’s rest becomes harder to achieve. The good news? A handful of simple, evidence‑based changes can turn those sleepless hours into real sleep. Below are the most effective strategies to tame night sweats, calm restless thoughts, and finally let your body recharge.
Why menopause throws sleep off balance
During menopause, hormone levels-especially estrogen and progesterone-fluctuate dramatically. These hormones interact with the brain’s sleep‑regulation centers, making it easier to drift into lighter stages of sleep or wake up frequently. In addition, the drop in estrogen can raise core body temperature, setting the stage for hot flashes that often strike in the evening.
Research from the North American Menopause Society shows that up to 80% of menopausal women report sleep disturbances, and about half describe them as severe enough to affect daily functioning.
Typical sleep‑disruptors in menopause
- Hot flashes Sudden waves of heat that can cause sweating, flushing, and a rapid heartbeat - usually hit between 6pm and midnight.
- Night sweats Excessive sweating during sleep that can soak clothing and sheets - a direct result of the body’s attempts to cool down.
- Increased anxiety or mood swings - hormone swings can amplify stress hormones, making it harder to fall asleep.
- Urinary urgency - the same hormonal changes can affect bladder control, prompting bathroom trips.
Identifying which of these is most disruptive for you helps tailor the right solution.
Lifestyle tweaks that actually work
Before reaching for medication, try these low‑risk adjustments. Consistency is key, so give each at least two weeks before deciding if it’s effective.
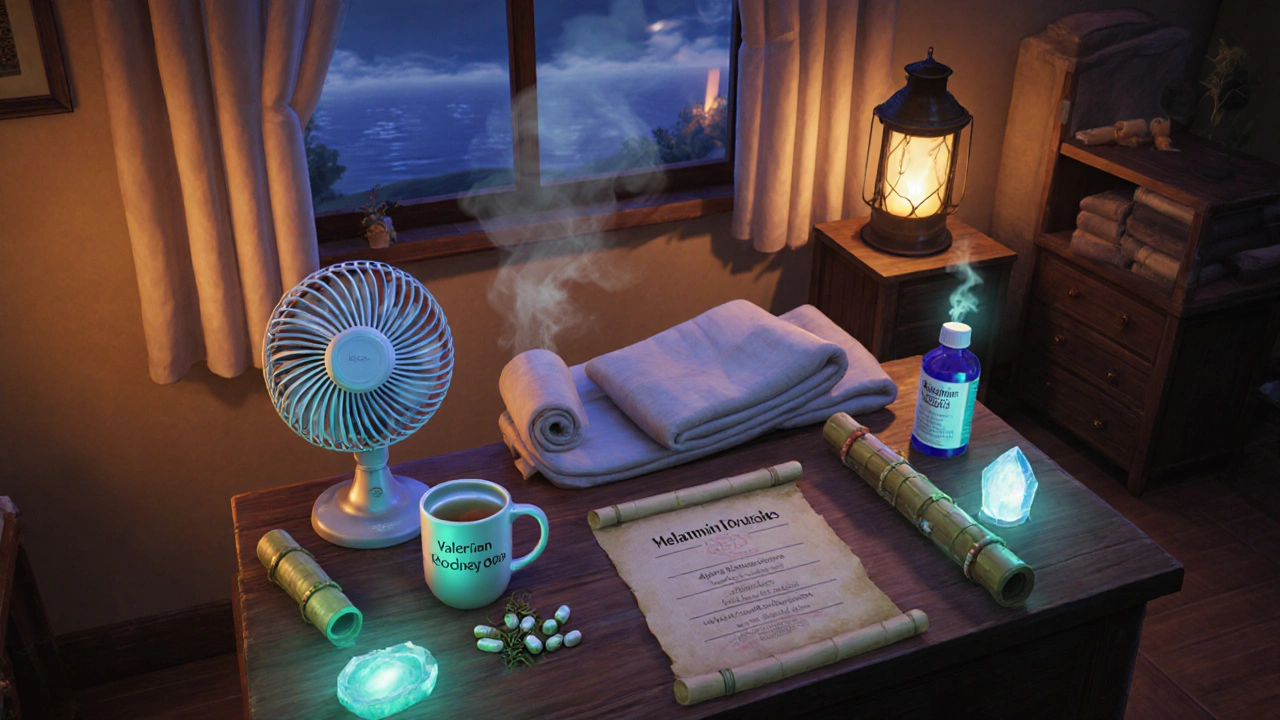
- Cool down the bedroom: Keep the room between 60‑67°F (15‑19°C). A fan or a portable AC unit can prevent overheating during a flash.
- Strategic timing of meals: Avoid heavy, spicy, or caffeine‑laden foods after 6pm. These can raise body temperature and trigger nighttime awakenings.
- Regular exercise-but not right before bed: Aim for 30 minutes of moderate activity (walking, swimming, yoga) most days. Finish at least three hours before bedtime to let the endorphin surge subside.
- Mind‑body calmers: Practicing deep‑breathing, progressive muscle relaxation, or a short guided meditation for 5‑10 minutes can lower cortisol, the stress hormone that spikes during menopause.
- Consistent sleep‑wake schedule: Go to bed and wake up at the same times daily, even on weekends. This trains the circadian rhythm and reduces the likelihood of fragmented sleep.
Food, drinks, and supplements that support sleep
What you sip and swallow matters. Certain nutrients can help modulate temperature and promote relaxation.
- Melatonin A hormone produced by the pineal gland that signals darkness to the brain - a low dose (0.5‑3mg) taken 30 minutes before bedtime can improve sleep onset, especially when natural production declines with age.
- Valerian root Herbal supplement known for mild sedative effects - 400‑900mg half an hour before sleep may reduce the time it takes to fall asleep without causing next‑day drowsiness.
- Magnesium (300‑400mg) - supports muscle relaxation and helps regulate body temperature.
- Phosphatidylserine - a lesser‑known nutrient that may blunt cortisol spikes when taken in the evening.
Always discuss supplements with a healthcare provider, especially if you’re on hormone therapy or other medications.
Hormone therapy and medical options
When lifestyle changes aren’t enough, medical interventions become a realistic next step.
Hormone therapy (HT) Treatment that replaces declining estrogen (with or without progesterone) to relieve menopausal symptoms has strong evidence for improving sleep quality by reducing hot flashes and night sweats. Low‑dose transdermal patches or gels tend to have fewer side effects than oral formulations.
For women who can’t use HT, options include:
- Selective serotonin reuptake inhibitors (SSRIs) - low‑dose escitalopram or paroxetine can lower the frequency of hot flashes.
- Cognitive‑behavioral therapy for insomnia (CBT‑I) - a structured, short‑term program that teaches sleep‑restriction, stimulus control, and cognitive reframing. Studies show CBT‑I can improve sleep efficiency by up to 20% in menopausal women.
Choosing the right route depends on your health history, personal preferences, and risk tolerance. A conversation with a gynecologist or menopause specialist will pinpoint the best plan.
Designing a sleep‑friendly bedroom
Environment plays a hidden but powerful role. Small changes can lower the chance of a night sweat turning into a full‑blown waking episode.
- Invest in breathable, moisture‑wicking bedding (cotton, bamboo, or linen). Avoid polyester blends that trap heat.
- Use lightweight, layered blankets that you can easily remove if you feel hot.
- Consider a white‑noise machine or a fan to mask sudden noises that could startle you awake.
- Limit light exposure: blackout curtains or a sleep mask block early‑morning sunlight that can disrupt melatonin release.
- Keep electronic devices out of the bedroom or use night‑mode settings to reduce blue‑light exposure at least an hour before sleep.
Sample bedtime routine for menopausal women
- 18:00 - Light dinner with lean protein, whole grains, and a side of leafy greens.
- 19:00 - 20‑minute gentle yoga session focused on deep breathing.
- 20:00 - Dim lights, switch off screens, and start a warm (not hot) shower.
- 20:30 - Take melatonin (if using) and any prescribed supplement.
- 20:45 - Write down any worries in a journal; set a “worry time” for the next day.
- 21:00 - Slip into breathable sleepwear, adjust bedroom temperature, and turn on a fan or white‑noise device.
- 21:15 - Lights out. If you can’t fall asleep after 20 minutes, get up and do a quiet activity (reading a paperback) until you feel sleepy.
Following a predictable sequence sends a clear signal to your brain that it’s time to shut down.
Comparison of common sleep‑aid options for menopausal women
| Option | How it works | Pros | Cons |
|---|---|---|---|
| Melatonin (supplement) | Signals darkness to the brain, helps reset circadian rhythm | Low cost, few side effects, works quickly | Effectiveness varies; may cause mild morning grogginess |
| Valerian root (herbal) | Mild GABA‑like activity promoting relaxation | Natural, non‑habit forming | Potential interaction with sedatives; taste can be off‑putting |
| Hormone therapy (HT) | Replaces declining estrogen, reducing hot flashes & night sweats | Addresses root cause; improves overall menopausal symptoms | Not suitable for everyone; requires medical supervision |
| CBT‑I (therapy) | Restructures thoughts & habits around sleep | Long‑term benefits; no medication needed | Requires time commitment and a trained therapist |
| Sleep‑environment tweaks | Reduces external triggers (heat, light, noise) | Zero cost after initial setup; lasting impact | May need trial‑and‑error to find optimal setup |
Frequently Asked Questions
Can night sweats be stopped without medication?
Yes. Cooling the bedroom, wearing breathable fabrics, staying hydrated, and limiting spicy or caffeine‑rich foods in the evening can reduce the frequency and intensity of night sweats for many women.
Is melatonin safe for long‑term use?
Low doses of melatonin are generally regarded as safe for several months. For longer use, discuss with your doctor to ensure it won’t interact with other treatments.
How soon can I expect improvement after starting hormone therapy?
Many women notice reduced hot flashes and better sleep within 2‑4 weeks, though full benefits may take up to three months.
What’s the difference between CBT‑I and regular talk therapy?
CBT‑I is a structured program focusing specifically on sleep habits, stimulus control, and cognitive restructuring. Traditional therapy addresses broader emotional issues but may not target sleep patterns directly.
Should I avoid alcohol before bed?
Yes. Alcohol can initially make you drowsy but later fragments sleep and may trigger night sweats, especially during menopause.
Next steps and troubleshooting
If you’ve tried the lifestyle tweaks and still wake up drenched or restless, consider the following ladder approach:
- Track your sleep. Use a journal or app to note when you experience flashes, what you ate, and bedtime habits. Patterns often reveal hidden triggers.
- Consult a menopause specialist. Bring your sleep log; they can recommend hormone therapy, low‑dose SSRIs, or refer you to a CBT‑I provider.
- Trial a supplement. Start with melatonin (0.5mg) for two weeks. If results are modest, add magnesium or valerian under guidance.
- Re‑evaluate your bedroom. If night sweats persist, invest in a cooling mattress pad or a moisture‑wicking pillow cover.
- Seek professional sleep testing. In rare cases, underlying sleep apnea can coexist with menopause, requiring a different treatment pathway.
Remember, every woman’s experience is unique. Combining a few of the strategies above usually yields the best outcome, letting you finally enjoy a night of uninterrupted, restorative sleep.
menopause sleep doesn’t have to be a nightly struggle. With the right mix of temperature control, smart nutrition, targeted supplements, and-when needed-medical guidance, you can reclaim your rest and wake up feeling refreshed.





Comments
Richard Sucgang
October 15, 2025 AT 12:15Your article, whilst comprehensive, neglects the lexical precision necessary for a discourse on nocturnal physiology. The phrase “night sweats” is ambiguous; a more accurate term would be diaphoresis. Moreover, the suggested temperature range fails to account for regional climatic variance. Consider integrating hygrometric data. The absence of a citation for the 80% statistic undermines credibility. Finally, the advice to “track your sleep” should be accompanied by a recommended methodology.
Russell Martin
October 15, 2025 AT 14:28Try adding a quick 5‑min stretch routine after dinner. It calms the nervous system and can lower those sudden hot flashes. Also, keep a glass of water bedside – staying hydrated helps regulate temp.
Jenn Zee
October 15, 2025 AT 16:58It is profoundly disheartening to witness the perpetuation of superficial remedies in the discourse surrounding menopausal sleep disturbances. One must first acknowledge that the physiological cascade triggered by estrogen decline is not a trivial inconvenience but a systemic transition worthy of rigorous scientific scrutiny. The article’s reliance on anecdotal suggestions, such as “use a fan,” betrays a lamentable paucity of engagement with the underlying neuroendocrine mechanisms. While the inclusion of melatonin and magnesium is commendable, the omission of dosage titration protocols reflects an incomplete pedagogical approach. Moreover, the casual reference to “light dinner” neglects the glycemic impacts of macronutrient composition on nocturnal thermoregulation. A truly erudite exposition would incorporate peer‑reviewed studies delineating the pharmacokinetics of valerian root in the context of hepatic metabolism. In addition, the guidance to “track your sleep” is rendered moot without an endorsement of validated actigraphy tools. The discourse further suffers from a lack of cultural sensitivity, ignoring the divergent experiences of women across ethnicities and socioeconomic strata. One cannot overlook the ethical imperative to present hormone therapy as a nuanced option rather than a binary proclamation. The suggestion to “avoid alcohol” skirts the broader issue of substance use patterns that may intersect with mental health comorbidities. The table comparing interventions, while visually appealing, fails to convey relative effect sizes, thereby impeding informed decision‑making. It is incumbent upon the author to elucidate the role of cognitive‑behavioral strategies beyond a bullet‑point mention, perhaps by outlining session frequency and therapeutic techniques. The narrative’s abrupt shift from lifestyle tweaks to medical options disrupts the logical flow expected of scholarly writing. Furthermore, the absence of discussion regarding sleep apnea prevalence in this demographic constitutes a glaring oversight. Finally, the article would benefit from a concluding synthesis that integrates the multifactorial nature of menopausal insomnia, rather than a perfunctory list of tips.
don hammond
October 15, 2025 AT 19:28Oh great, another endless lecture on hormone drama 🙄💤. As if we needed more buzzwords and charts to feel validated.
Ben Rudolph
October 15, 2025 AT 21:58While your grammar crusade is noted, the real issue is that many women still suffer night sweats despite perfect syntax.
Ian Banson
October 16, 2025 AT 00:28Honestly, British women have never complained about menopausal insomnia the way our American sisters do – perhaps it’s the climate, perhaps it’s the tea.
marcel lux
October 16, 2025 AT 02:58I appreciate your perspective, but in my experience even a modest fan can make a night of difference. Let’s keep sharing what works.
Charlotte Shurley
October 16, 2025 AT 05:28The emphasis on breathable bedding is especially valuable; many overlook how fabric choice directly influences skin temperature.
Steph Hooton
October 16, 2025 AT 07:58Indeed, the recommendation to limit caffeine after six is both prudent and evidence‑based. I would add that even decaffeinated coffee can contain trace stimulants, so be mindful.
RUCHIKA SHAH
October 16, 2025 AT 10:28Sleep is a simple yet complex thing – when the body cools, the mind can finally let go. Small habits matter more than grand plans.
Justin Channell
October 16, 2025 AT 12:58Exactly! 😊 Start with a short breathing exercise and you’ll feel the difference. Consistency is the secret sauce.
Basu Dev
October 16, 2025 AT 15:28From a clinical standpoint, it is essential to differentiate between primary insomnia and sleep disruption secondary to vasomotor symptoms. When evaluating a patient, begin with a comprehensive history that includes the frequency, intensity, and timing of hot flashes. Correlate these with sleep logs to identify patterns that may be mitigated by environmental adjustments. In cases where lifestyle modifications prove insufficient, consider a low‑dose transdermal estrogen patch, as it offers stable serum levels with fewer hepatic effects. For those contraindicated for hormone therapy, a selective serotonin reuptake inhibitor such as low‑dose paroxetine has demonstrated efficacy in reducing nocturnal awakenings. Additionally, magnesium supplementation can be introduced gradually, monitoring for gastrointestinal tolerance. Finally, referral to a certified sleep therapist for CBT‑I can provide patients with lasting behavioral tools to improve sleep architecture.
Krysta Howard
October 16, 2025 AT 17:58Great rundown! 👍 However, remember that supplements aren’t a one‑size‑fits‑all solution – always check interactions with any meds you’re on before adding new pills.
Elizabeth Post
October 16, 2025 AT 20:28Thanks for the thorough guide – I’ll try the cooling pillow cover this week.
Brian Latham
October 16, 2025 AT 22:58These tips are decent but sound like the usual internet fluff – could use more solid data.
Barbara Todd
October 17, 2025 AT 01:28Is there any real study backing the fan recommendation?