Psoriatic Arthritis: How Skin Disease Turns Into Joint Pain

When your skin breaks out in red, scaly patches, it’s easy to think it’s just a skin problem. But for about 1 in 3 people with psoriasis, something deeper is happening - their joints are starting to hurt, swell, and stiffen. This isn’t just coincidence. It’s psoriatic arthritis, a condition where the same immune system that attacks the skin starts attacking the joints too.
It’s Not Just Psoriasis - It’s a Systemic Problem
Psoriatic arthritis doesn’t show up out of nowhere. It’s the body’s immune system going off-track. In psoriasis, immune cells rush to the skin and cause inflammation, leading to those thick, flaky plaques. But in psoriatic arthritis, those same immune cells turn on the joints, tendons, and even the places where tendons attach to bone. That’s why you can have flaky elbows and swollen fingers at the same time. Most people develop psoriasis first - usually between ages 15 and 35. Then, years later, joint pain creeps in. About 70% of the time, joint symptoms show up 5 to 10 years after skin symptoms. But here’s the twist: in 15% of cases, the joints hurt before the skin ever breaks out. That’s why so many people go years without the right diagnosis. They see a dermatologist for their skin, a GP for their aching knee, and nobody connects the dots.The Five Ways Psoriatic Arthritis Shows Up
This isn’t one single disease. It’s five different patterns, and each one looks different.- Asymmetric oligoarthritis - the most common form. It hits just a few joints, but not the same ones on both sides. Maybe your left knee and right wrist. It’s unpredictable, and it’s often mistaken for regular joint wear and tear.
- Symmetric polyarthritis - this one looks like rheumatoid arthritis. Joints on both sides swell together - both hands, both ankles. But unlike RA, psoriatic arthritis rarely tests positive for rheumatoid factor.
- Distal interphalangeal predominant (DIP) - this one targets the joints closest to your fingernails. If you’ve got pitted nails and stiff fingertips, this is likely the culprit. It’s rare in other types of arthritis.
- Spondylarthritis - your spine gets involved. Lower back pain that’s worse in the morning and improves with movement? That’s a classic sign. It can also affect the sacroiliac joints, making it hard to stand up straight after sitting for too long.
- Arthritis mutilans - the rarest and most destructive. Less than 5% of people get this, but it eats away at bone. Fingers can shorten. Joints collapse. It’s called the “opera glass hand” because the fingers look like they’ve been squeezed through a lens.
The Silent Clues: Nail Changes and Swollen Digits
Your nails can tell you more than you think. If you’ve got pitting - tiny dents like someone tapped them with a pin - that’s a red flag. So is when your nail lifts off the nail bed (onycholysis), or turns yellow-brown. About 80% of people with psoriatic arthritis have these nail changes. And if you see them before the joints hurt? That’s a strong hint. Then there’s dactylitis - or “sausage digits.” One finger or toe swells up completely, looking like a little sausage. It’s not just the joint. It’s the whole digit - tendons, skin, and joint all inflamed together. About half of people with psoriatic arthritis get this. It’s so specific that doctors use it to rule out other kinds of arthritis. And don’t ignore where your tendons attach to bone. That’s called enthesitis. It’s the Achilles tendon at the back of your heel. It’s the bottom of your foot - plantar fasciitis that doesn’t go away. It’s the elbow, the hip, even the ribs. These aren’t random pains. They’re signals from your immune system.How It’s Different From Other Arthritis
Osteoarthritis? That’s wear and tear. Cartilage breaks down over time. No inflammation. No swelling. Just stiffness and creaking. Psoriatic arthritis? It’s active, burning inflammation. Your joints get hot, red, and swollen. You feel exhausted. Your body is fighting something. Rheumatoid arthritis (RA) often looks similar - symmetric joint swelling, morning stiffness. But RA almost always shows up with a positive rheumatoid factor blood test. Psoriatic arthritis? That test is negative. And RA doesn’t cause dactylitis or enthesitis. It doesn’t cause nail pitting. It doesn’t usually affect the spine the same way. Even the X-rays look different. In psoriatic arthritis, you might see “pencil-in-cup” deformities - where one bone erodes into the shape of a pencil and fits into a cup-like depression in the next bone. You might also see new bone growing where tendons attach - called “whiskering.” That’s unique to psoriatic arthritis and other spondyloarthropathies.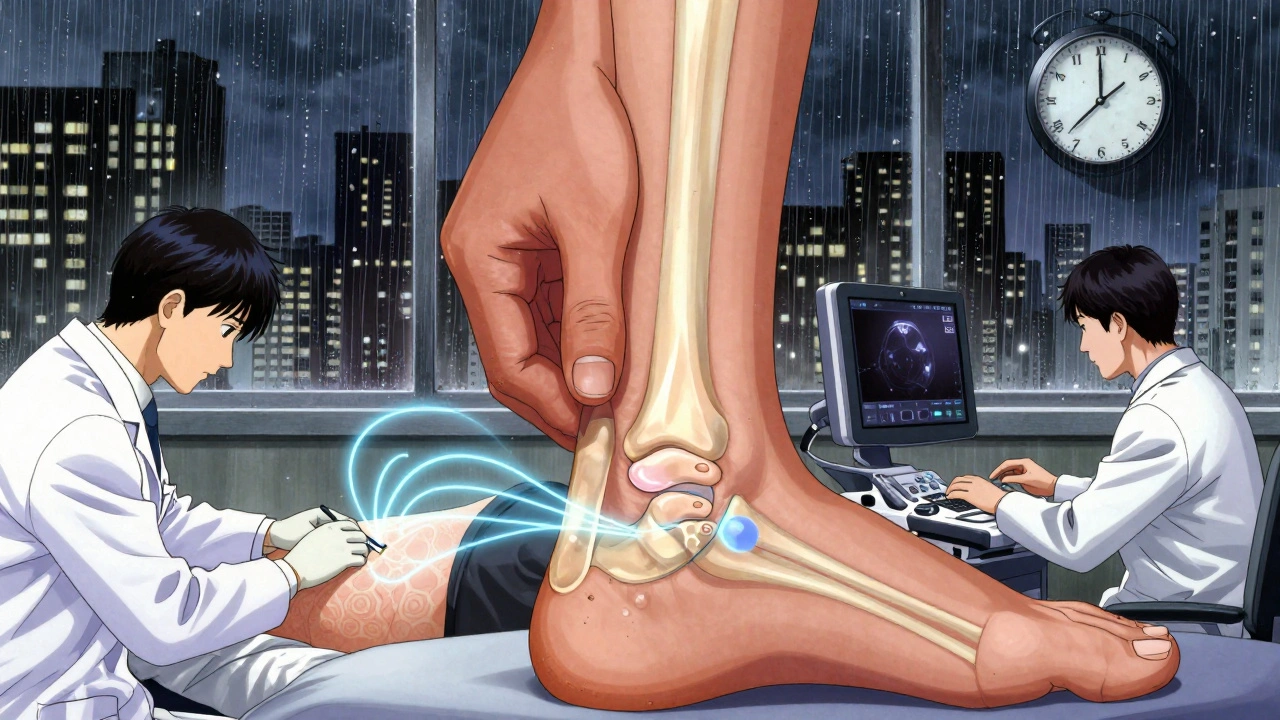
Why Diagnosis Takes So Long - And Why It Matters
The average person waits 2 to 5 years to get diagnosed. Many see three or more doctors. Why? Because the symptoms are scattered. A dermatologist sees the skin. A GP sees the knee pain. A podiatrist sees the heel. Nobody puts it together. And the cost of waiting? It’s huge. Studies show that if you wait more than 6 months after symptoms start, you’re 3 times more likely to have permanent joint damage by the time you’re diagnosed. By 12 months? The damage accelerates. Joints can erode. Bones can fuse. Mobility can vanish. The key? Look for the combo: psoriasis + joint pain + nail changes + dactylitis. If you have two or more of those, you need to see a rheumatologist - not wait for your skin to get worse.What Actually Helps - And What Doesn’t
Treatment has changed dramatically in the last decade. It’s not just about painkillers anymore.- DMARDs like methotrexate are still used - especially early on. But they only work for about half of people.
- TNF inhibitors - drugs like adalimumab and etanercept - are the first-line biologics. They reduce inflammation fast. About 65% of people reach minimal disease activity within 6 months.
- IL-17 and IL-23 inhibitors - newer drugs like secukinumab and guselkumab - are even more targeted. They block specific parts of the immune system that drive both skin and joint inflammation. In one trial, 64% of patients had a 50% improvement in joint symptoms after just 6 months.
What Triggers Flares - And How to Manage Them
You can’t control your immune system, but you can control some triggers.- Stress - cited by 85% of patients. Emotional stress, work pressure, grief - they all spark flares.
- Infections - especially strep throat. It’s linked to a 1.8 times higher chance of psoriatic arthritis developing.
- Cold weather - 57% of people report worse symptoms in winter. Dry air, less movement, less sunlight - all play a role.
- Obesity - carrying extra weight doesn’t just strain your joints. Fat tissue releases inflammatory chemicals. People with a BMI over 30 are more than twice as likely to develop psoriatic arthritis.

Coordinated Care Is the Game-Changer
This isn’t a skin doctor’s problem or a rheumatologist’s problem. It’s both. When dermatologists and rheumatologists work together, outcomes jump from 54% to 82% effectiveness. Why? Because they see the full picture. The dermatologist notices new nail changes. The rheumatologist spots early enthesitis on ultrasound. Together, they catch it before the damage spreads. Regular monitoring matters too. Tools like the MASES score (for enthesitis), the Dactylitis Count, and the NAPSI (for nail severity) help track progress - not just how you feel, but what’s really happening inside.The Future: Personalized Treatment Is Coming
By 2027, treatment may be guided by your genes and proteins - not just your symptoms. Researchers are already testing blood tests that predict who will respond to which drug. One study showed that patients with certain biomarker profiles had a 40% higher chance of achieving remission with the right targeted therapy. The goal? Not just to slow damage - but to stop it before it starts. Early intervention within 6 months of symptoms cuts radiographic progression by 73% over two years. That’s not a small win. That’s life-changing.What You Should Do Right Now
If you have psoriasis and you’ve had joint pain for more than a few weeks - especially if it’s worse in the morning, if your nails are changing, or if a finger or toe is swollen like a sausage - don’t wait. Ask your dermatologist for a referral to a rheumatologist. Bring a list: when the pain started, which joints hurt, what makes it better or worse, whether your nails are changing. Take a photo of your skin and nails if you can. You don’t need to live with this pain. The treatments exist. The science is there. The only thing missing is the step you take next.Can psoriatic arthritis develop without skin psoriasis?
Yes, in about 15% of cases, joint symptoms appear before any visible skin psoriasis. This makes diagnosis harder, but if you have dactylitis, enthesitis, nail changes, or a family history of psoriasis, rheumatologists can still identify psoriatic arthritis through imaging and blood tests.
Is psoriatic arthritis the same as rheumatoid arthritis?
No. Rheumatoid arthritis (RA) is symmetric - it affects the same joints on both sides - and usually tests positive for rheumatoid factor. Psoriatic arthritis is often asymmetric, rarely has a positive rheumatoid factor, and is linked to skin and nail changes, dactylitis, and enthesitis - none of which are typical in RA.
Can psoriatic arthritis be cured?
There’s no cure yet, but it can be controlled. With early treatment using biologics or targeted therapies, many people reach minimal disease activity - meaning little to no pain, swelling, or fatigue. The goal is to stop joint damage before it happens.
Does weight loss help with psoriatic arthritis?
Yes. Losing even 5% of your body weight reduces inflammation and improves how well medications work. Fat tissue produces inflammatory chemicals, so carrying extra weight makes psoriatic arthritis harder to control. Weight loss is one of the most effective non-drug treatments.
What’s the best test to diagnose psoriatic arthritis?
There’s no single test. Diagnosis combines physical exam, blood tests (to rule out RA), imaging (X-rays, ultrasound, or MRI to spot enthesitis or bone changes), and clinical signs like nail pitting, dactylitis, and psoriasis history. The 2023 ACR/EULAR criteria now include imaging findings and biomarkers for higher accuracy.
Are biologics safe for long-term use?
Biologics are generally safe for long-term use, but they require monitoring. They can increase the risk of infections and, in rare cases, certain cancers. JAK inhibitors carry a slightly higher risk of heart events. Your doctor will screen you for TB, hepatitis, and other conditions before starting treatment and monitor you regularly.






Comments
Gene Linetsky
December 3, 2025 AT 07:09Let me guess - Big Pharma paid these doctors to write this. You think psoriatic arthritis is just some random immune glitch? Nah. It’s the glyphosate in your food, the 5G towers near your house, and the fluoridated water they’ve been pumping into your tap since birth. The skin? That’s your body’s alarm system. The joints? The cover-up. They don’t want you to know it’s all about toxins. Get off the meds. Do a 30-day juice cleanse. You’ll thank me later.
Ignacio Pacheco
December 3, 2025 AT 12:32So let me get this straight - you’re telling me the same immune cells that give me scaly elbows also turn my knuckles into overcooked hot dogs? Cool. So basically my body’s got a case of ‘I hate myself today’ and it’s taking it out on my joints. Thanks, biology. I’ll be over here, staring at my sausage fingers like they’re a weird art installation.
Jim Schultz
December 4, 2025 AT 21:08Let’s not pretend this is science - it’s a marketing brochure for biologics. You cite ‘65% response rates’ like that’s a cure, not a 35% failure rate. You mention ‘pencil-in-cup’ deformities like they’re a fun fact, not a warning sign that your bones are being eaten alive. And you completely ignore the fact that 70% of patients on TNF inhibitors develop secondary failure within 2 years. This isn’t education - it’s a sales pitch with footnotes.
Also, ‘losing 5% weight helps’? That’s like saying ‘drinking water helps you not drown.’ Groundbreaking.
Kidar Saleh
December 5, 2025 AT 09:27In the UK, we call this the ‘invisible illness trap’ - you’re too young for arthritis, too healthy-looking for disability, and your GP says ‘it’s just stress.’ I waited three years before a rheumatologist spotted the dactylitis in my toe. My nail pitting? ‘Oh, you’re just a nail-biter.’ The system isn’t broken - it’s designed to ignore people like us until it’s too late. Thank you for naming the signs. Someone needed to say this out loud.
Chloe Madison
December 6, 2025 AT 08:41PLEASE. If you have psoriasis and your knees feel like they’re filled with wet cement in the morning - GO TO A RHEUMATOLOGIST. TODAY. Not next week. Not after your vacation. TODAY. I was told it was ‘just aging’ at 29. By 31, I had permanent joint damage. I’m on biologics now. I can walk. I can hold my coffee. I can hug my kids without wincing. It’s not magic - it’s timing. You have a 6-month window. Don’t waste it. You’re not ‘just tired.’ You’re not ‘overdoing it.’ Your body is screaming. Listen.
Vincent Soldja
December 7, 2025 AT 10:13Psoriatic arthritis is real. Treatment options exist. Early referral improves outcomes. End of discussion.
Makenzie Keely
December 9, 2025 AT 01:40Thank you for writing this with such precision - especially the part about enthesitis being mistaken for plantar fasciitis. I had heel pain for two years. Two podiatrists. Two cortisone shots. One MRI. And then, finally, a rheumatologist noticed the tiny dents in my nails and asked, ‘Do you have psoriasis?’ I didn’t even know I had it - it was just a little flakiness on my scalp. Now I know: it’s not just skin. It’s a whole-body signal. If you have psoriasis and any unexplained joint or tendon pain - don’t wait. Bring this article to your doctor. Print it. Highlight it. Demand a referral. Your future self will cry tears of relief.
James Kerr
December 9, 2025 AT 06:55Yeah, I’ve got the nail pitting and the swollen toe. Took me a year to connect the dots. Now I’m on a biologic and I can actually play with my dog again. No drama, no hype - just got help before it got worse. You’re not alone. And it’s not ‘just old age.’
👍