Severe Hypoglycemia and Hyperglycemia from Diabetes Medications: Emergency Care Protocols

Diabetes Emergency Checker
Check Your Blood Sugar Emergency Risk
Enter your current blood glucose level and ketone status to determine if you need immediate medical attention.
Enter values to see emergency assessment
What Counts as a Diabetes Emergency?
When your blood sugar drops too low or spikes too high, it’s not just uncomfortable-it’s dangerous. Severe hypoglycemia means your blood glucose is below 54 mg/dL (3.0 mmol/L) and you can’t treat yourself. You need someone else to step in. Severe hyperglycemia isn’t just a high number-it’s diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS), both of which can kill you if not treated fast. DKA usually shows up with blood sugar over 250 mg/dL, ketones in your blood, and acid in your system. HHS hits even harder: sugar levels above 600 mg/dL, extreme dehydration, and thick, syrupy blood. These aren’t minor blips. They’re medical crises that demand immediate action.
Glucagon: Your Lifeline for Low Blood Sugar
If you’re on insulin and your blood sugar crashes, glucagon is the only thing that can save you when you’re unconscious or too confused to swallow. For years, the only option was a messy kit: freeze-dried powder, a syringe, mixing it up, then injecting. Most people never learned how. A 2021 study found only 42% of caregivers could use it right. That’s why new forms changed everything. Baqsimi is a nasal spray-just stick it in one nostril and press. Gvoke is a ready-to-use autoinjector like an EpiPen. Both work in under 15 minutes. No mixing. No needles. No panic. The FDA approved Baqsimi in 2019 and Gvoke in late 2019. Now, 85% of endocrinologists recommend these over the old kit. They’re easier, faster, and more reliable. If you’re on insulin, you need one. Not someday. Now.
What Happens If You Give Glucagon to Someone With High Blood Sugar?
It’s a deadly mistake. Glucagon raises blood sugar. If someone is in DKA or HHS, their body is already drowning in glucose and ketones. Giving glucagon makes it worse. It can push them into coma or cardiac arrest. On the flip side, giving insulin to someone with severe hypoglycemia is just as bad. It drops their sugar even lower. You can’t guess. You have to know. If someone is unconscious, don’t assume it’s low sugar. Don’t give insulin. Don’t pour juice down their throat. Call 911. If you have a glucose meter, check it. If you don’t, and you’re not 100% sure, wait. Administer glucagon only if you’re certain it’s hypoglycemia. The American Diabetes Association says: if you can’t measure, don’t medicate. Better to wait than to kill.
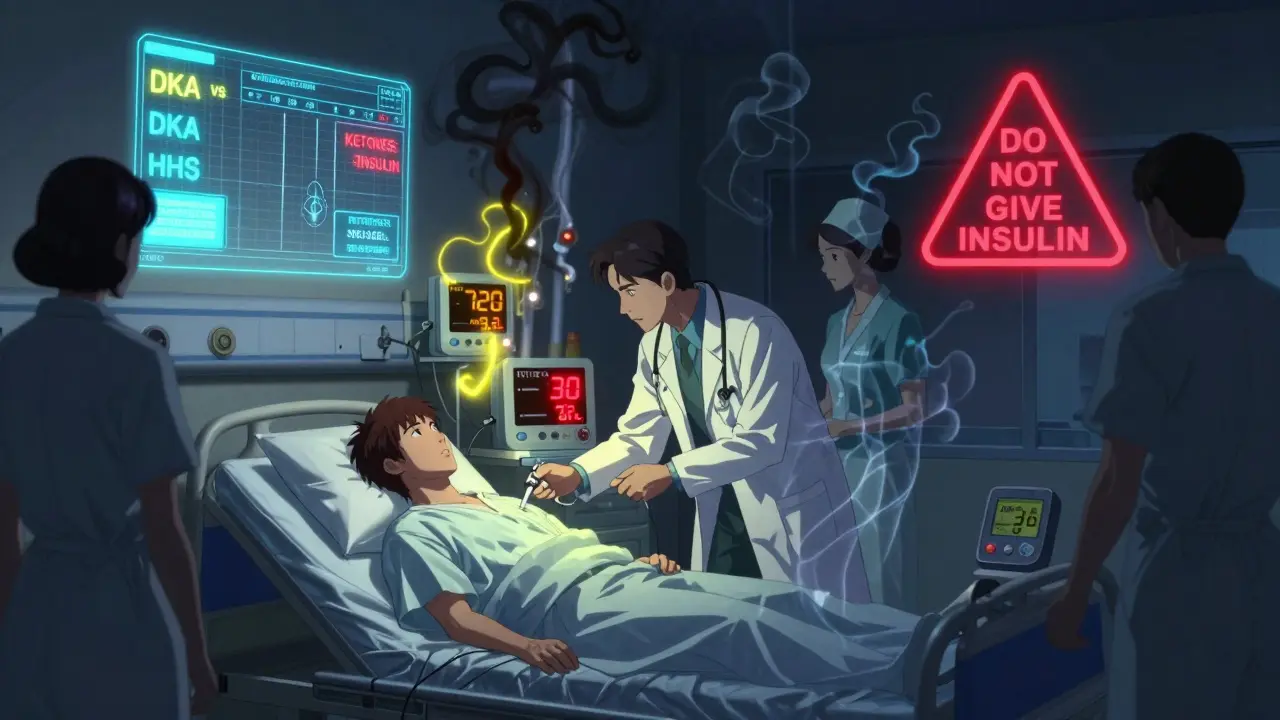
How to Treat High Blood Sugar Emergencies
Hyperglycemic emergencies don’t respond to pills or insulin shots at home. They need hospital care. The goal is threefold: rehydrate, replace electrolytes, and lower sugar slowly with IV insulin. First, fluids-usually 1 to 2 liters of saline in the first hour. Then, potassium. When insulin starts working, it drives potassium into cells. If your levels are already low, you can crash. Doctors add 20-30 mEq of potassium chloride to the IV drip. Insulin goes in as a steady IV drip-not a bolus. Too much too fast can cause brain swelling. For mild DKA (pH above 7.0), some doctors now use fast-acting insulin like lispro under the skin, but only if the patient is alert and stable. For severe cases, IV is still the rule. Blood ketone testing is now standard in ERs. If your ketones are above 1.5 mmol/L, go to the hospital. Don’t wait. Don’t try to “tough it out.”
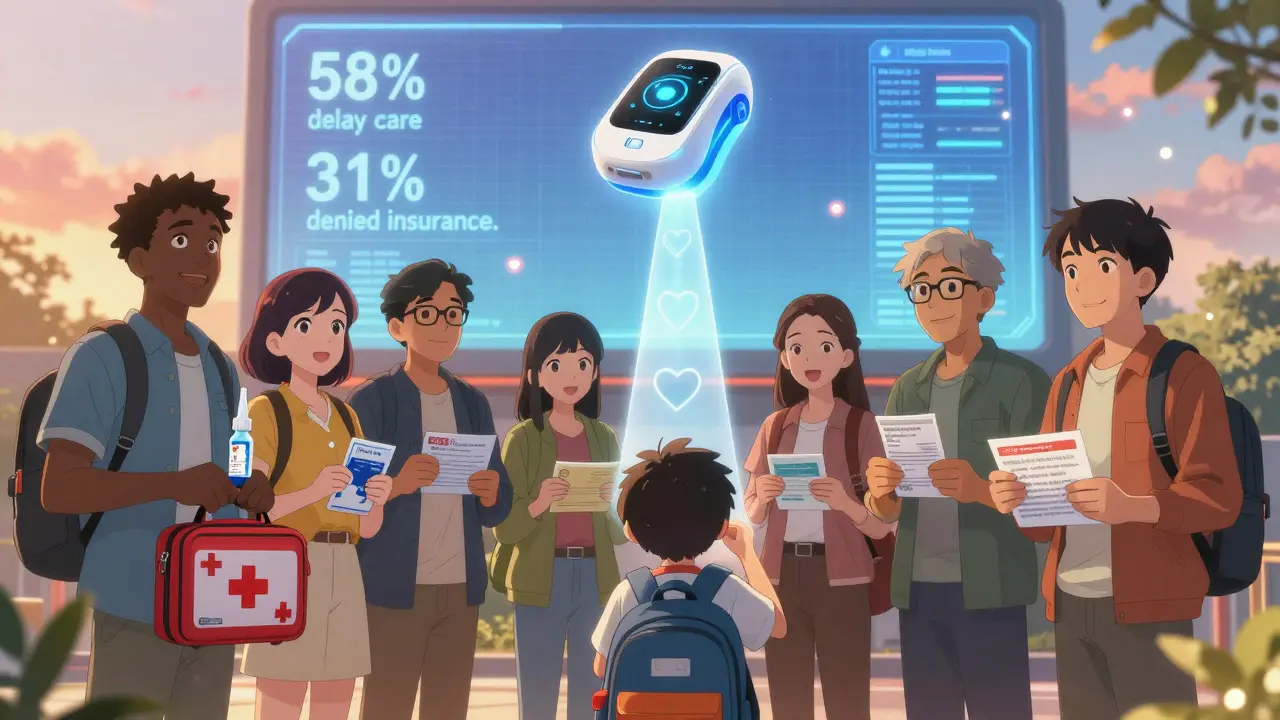
Why People Delay Treatment-And What You Can Do
A T1D Exchange survey found that 58% of people wait more than 12 hours before seeking help during a hyperglycemic crisis. Why? They think it’s just “a bad day.” They don’t recognize the early signs: extreme thirst, frequent urination, nausea, fruity breath, confusion. Others fear the hospital. Or they don’t have a plan. A 2022 Beyond Type 1 survey showed 63% of type 1 patients had experienced severe low blood sugar, but only 41% always carried glucagon. Fear of using it wrong was the top reason. Training fixes this. A 30-minute video can boost successful glucagon use from 32% to 89%. Practice quarterly with a training device. Keep your kit in your bag, your car, your child’s backpack. Label it. Teach your partner, your kids, your coworker. Make it normal. If your school nurse refuses to use glucagon, get a written emergency plan. You have rights.
What Should Be in Your Emergency Kit?
Forget the old-school glucagon kit unless you’re trained and willing to practice. Go for the nasal spray or autoinjector. Your kit should include: one ready-to-use glucagon device (check expiration date), glucose tablets (4g each-exactly 15g for mild lows), a small bottle of regular soda (not diet), a glucose meter with extra strips, ketone test strips, and a printed emergency card with your name, diagnosis, insulin type, emergency contacts, and doctor’s number. Keep it in your purse, your car, your child’s backpack. Check it every three months. Expired glucagon won’t work. Wet strips give false readings. Replace what’s old. Don’t wait for a crisis to find out your kit is useless.
What’s New in 2025?
The biggest breakthrough isn’t a drug-it’s a system. The Beta Bionics iLet, a dual-hormone artificial pancreas, got FDA approval in 2023. It automatically delivers tiny doses of glucagon when it predicts a low. In trials, it cut severe hypoglycemia by 72%. But it’s not widely available yet-only 12 U.S. centers offer it. Still, it’s the future. Companies like Eli Lilly now link glucagon devices to apps. The Gvoke HelperApp walks you through each step with video. It even reminds you to replace your device before it expires. In 2025, expect more integration: CGMs that auto-alert 911, smart pens that track insulin use, and insurance plans that cover glucagon without prior authorization. But for now, the best tool is still knowledge. Know your numbers. Know your signs. Know how to use your glucagon. That’s what saves lives.
Who’s at Risk-and Why It’s Not Fair
Black and Hispanic patients with diabetes are 2.3 times more likely to be hospitalized for severe hypoglycemia than white patients. Why? Access. Cost. Education. Medicaid patients face prior authorization for glucagon 31% of the time. Private insurance? Only 12%. The new glucagon devices cost $250-$270. The old kit is $130-but if you can’t use it, it’s useless. Insurance won’t cover it if you’re on Medicare Part D and don’t have a prescription on file. You need to ask for it. Demand it. If your doctor says, “You probably won’t need it,” push back. The ADA says: everyone on insulin should have glucagon. Period. If you’re on SGLT2 inhibitors like Farxiga or Jardiance, you’re at risk for DKA even with normal blood sugar. Know the signs. Test for ketones if you’re sick. Don’t wait. This isn’t just about medicine. It’s about justice. Your life matters. Your access should too.






Comments
Evan Smith
January 8, 2026 AT 16:15I had no idea glucagon was this easy now. I used to carry the old kit and always forgot how to mix it. Just last month my buddy passed out at the BBQ and I used Baqsimi-no mess, no panic. He woke up five minutes later like nothing happened. Why isn't this in every school and workplace?
Lois Li
January 9, 2026 AT 13:50This is the most important post I've read all year. I'm a nurse and I've seen too many people wait too long because they thought it was just 'a bad day.' The part about ketones above 1.5 mmol/L needing ER care? That should be on every diabetes app. Please share this with everyone you know.
Annette Robinson
January 9, 2026 AT 14:22I’m a parent of a child with type 1. We’ve had two DKA episodes in the last year. The hospital staff didn’t even know how to explain ketone strips to us. This post? It’s everything. I printed it out and gave copies to the school nurse, my sister, and my neighbor. If you’re on insulin, you need to read this. No excuses.
Luke Crump
January 9, 2026 AT 15:02Let me ask you this: if we’re so afraid of giving glucagon to someone with high sugar, why are we still letting pharmaceutical companies sell insulin like candy? Who decided that the body’s natural balance is less important than a $300 vial? We’re treating symptoms like they’re sins. This isn’t medicine-it’s capitalism with a stethoscope.
Manish Kumar
January 10, 2026 AT 04:46You know, in India, many people with diabetes don't even have access to glucose meters, let alone nasal glucagon. I’ve seen patients use sugar packets from tea stalls to treat lows, and when that fails, they just sit and wait. The irony is that the same people who can’t afford glucagon are the ones who work 12-hour shifts without breaks, skipping meals because they’re afraid of lows. Technology is amazing, but if the system doesn’t change, we’re just putting band-aids on a hemorrhage.
Molly Silvernale
January 11, 2026 AT 23:20I used to think DKA was just... bad sugar. But now? I see it as the body screaming-screaming in acetone breath, in trembling hands, in a mind that can’t remember its own name. And glucagon? It’s not a drug. It’s a lifeline thrown by someone who didn’t give up on you. I carry mine in my bra. Yeah, I said it. Better than losing it in a purse. And I’ve trained my cat. (She’s not helpful. But she knows the bag.)
Kristina Felixita
January 13, 2026 AT 14:30I’m so glad this was posted. My mom is on SGLT2 inhibitors and she thought ketones only happened with high sugar. She got DKA last winter with a blood sugar of 180. No one told her. She almost didn’t make it. Now she tests ketones every time she’s sick. I got her the Gvoke autoinjector and we practice every Sunday. It’s not weird. It’s survival.
Joanna Brancewicz
January 14, 2026 AT 00:57Glucagon access disparities are a public health crisis. Medicaid prior auth delays = preventable hospitalizations. Data: 31% vs 12%. This isn’t policy. It’s negligence.
christy lianto
January 16, 2026 AT 00:18I used to think I was invincible. I didn’t carry glucagon. I thought I’d ‘just wake up.’ I passed out in the parking lot last year. My coworker used my expired kit. I woke up in the ER. Now I have two Baqsimi sprays. One in my car. One in my gym bag. I don’t care what you think. I’m alive because someone didn’t hesitate. Don’t be the person who waits.
Ken Porter
January 16, 2026 AT 04:55Why are we spending millions on nasal glucagon when we could just teach people to eat a candy bar? This is over-engineered. People in the 80s didn’t have this stuff and they lived. America’s obsession with making everything idiot-proof is just making us lazy.