Acid indigestion: quick relief, prevention, and when to see a doctor
Feel that burning under your breastbone after a big meal? That’s acid indigestion (heartburn) — and it’s more than annoying. Up to 30% of adults get it regularly. This page gives fast fixes you can try now, simple habits that cut flare-ups, and clear red flags that mean you need medical help.
First, the easiest relief you can try at home: chew sugar-free gum for 30 minutes after eating to boost saliva and wash acid down; take an over-the-counter antacid (calcium carbonate or magnesium hydroxide) for immediate neutralizing; or use an H2 blocker like ranitidine alternative options if you need longer relief. If you use antacids often, talk to a pharmacist — they can interact with other meds and hide bigger problems.
Practical prevention tips that actually work
Skip the guesswork. Key triggers are fatty or fried foods, citrus, chocolate, peppermint, coffee, and alcohol. Eat smaller portions and stop eating 2–3 hours before lying down. Raise the head of your bed 6–8 inches if you get night symptoms. Lose even a little weight if you’re overweight — many people feel fewer flare-ups after dropping 5–10 pounds. Quit smoking; it weakens the valve between stomach and esophagus.
Watch what you drink: swapping a morning coffee for low-acid options or tea can help. Tight clothes and heavy lifting right after meals force acid upward — change those habits. Also check medications: NSAIDs, some blood pressure drugs, and certain supplements can worsen reflux. If you’re on long-term meds, ask your prescriber whether they might be a factor.
When acid indigestion needs a doctor
See a doctor right away for sudden, severe chest pain, shortness of breath, or sweating — those can be heart-related. Book an urgent appointment if you notice trouble swallowing, unexplained weight loss, persistent vomiting, vomiting blood, or black tarry stools. If you rely on antacids more than twice a week for months, you may have GERD and should discuss stronger options like a proton pump inhibitor (for example, esomeprazole, sold as Nexium) and evaluation to rule out complications.
If you have diabetes, take blood-thinning drugs, or are pregnant, mention acid symptoms to your provider sooner. Tests such as endoscopy or pH monitoring might be advised for frequent or severe cases.
Want a practical next step? Start a 2-week diary: note what you eat, when symptoms start, and what helps. That data makes conversations with your doctor or pharmacist faster and more useful. For gentle long-term control, combine diet fixes, sleep changes, and weight management before jumping to daily medication unless your clinician recommends it.
If you’d like, check our Nexium guide for details on PPIs and safe use, or browse our posts on nausea, antacid alternatives, and online pharmacy safety to learn where to buy treatments and how to use them safely.
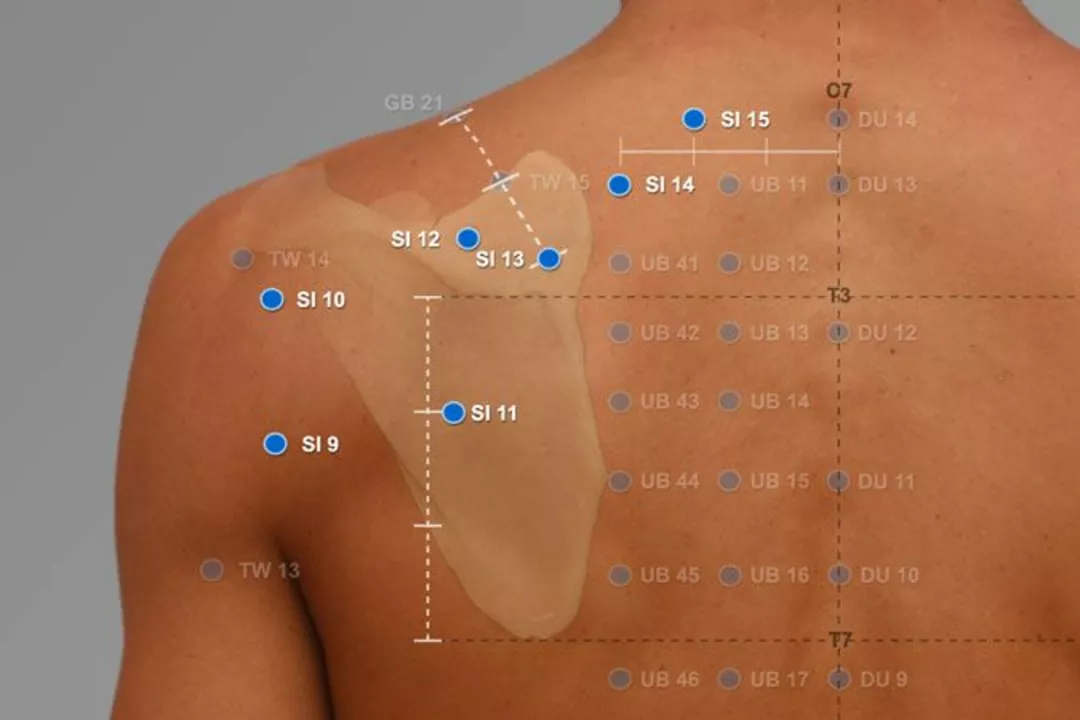
The Benefits of Acupuncture for Acid Indigestion Relief
As someone who has personally experienced the discomfort of acid indigestion, I can't recommend acupuncture enough for relief. Not only does it help to reduce inflammation in the stomach, but it also aids in promoting a healthy digestive system. Acupuncture has been proven to stimulate the release of endorphins, which helps to relax the body and reduce stress, a common trigger for indigestion. The treatment is non-invasive and has minimal side effects, making it a safe and effective option for those suffering from acid indigestion. Give acupuncture a try and experience the relief it can bring to your digestive system.