Brand-Name Medications: What They Are, Why They Cost More, and How to Navigate Them
When you pick up a prescription, you might see the name of a drug like Calan, a brand-name calcium channel blocker used for high blood pressure and heart rhythm issues—not its generic version, verapamil. Brand-name medications, are drugs first developed and marketed by pharmaceutical companies under a patent-protected name. These are the ones you see advertised on TV, promoted by reps, and often prescribed first. But behind that familiar label is the same active ingredient found in cheaper generics. The difference isn’t in how they work—it’s in the cost, the branding, and the timing of when they hit the market.
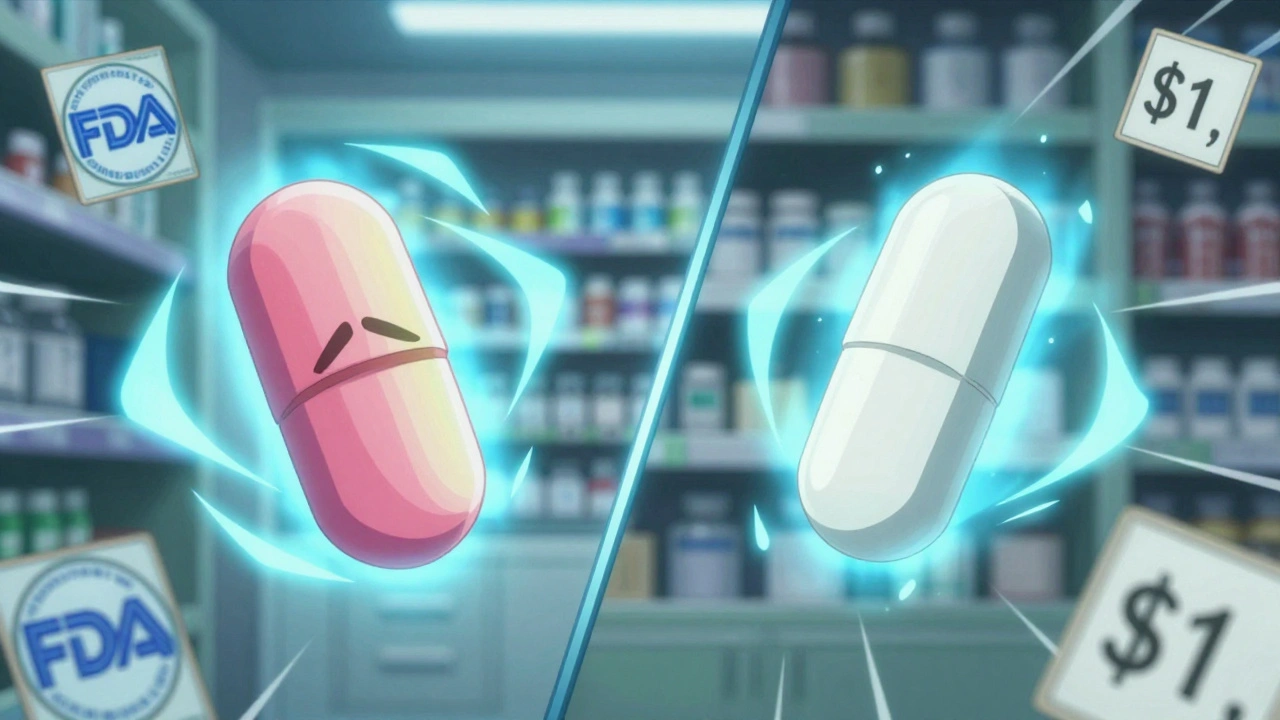
Why does this matter? Because generic drugs, are FDA-approved copies of brand-name medications that must meet the same strict standards for safety, strength, and effectiveness. The FDA requires them to deliver the same result in your body—no exceptions. Yet many people still believe brand-name versions are superior. That’s not true. What’s true is that brand-name drugs cost 80% to 85% more, mostly because the company paid millions to develop the drug, run clinical trials, and market it. Once the patent expires, other manufacturers can make the same drug, and prices drop fast. But not everyone switches. Some doctors still default to brand names. Some pharmacies stock them first. And some patients just stick with what they know.
That’s where FDA approval, the rigorous process that ensures every drug—brand or generic—is safe and effective before it reaches you becomes your safety net. Every pill you take, whether it’s brand-name medications or their generic twins, has been reviewed by the FDA. The process for generics isn’t easier—it’s smarter. They don’t need to repeat expensive clinical trials because they’re proven to be bioequivalent. That’s why you can safely switch from brand-name Lamictal to generic lamotrigine, or from brand-name Bactrim to its generic TMP-SMX. But knowing that doesn’t always make it easy. Drug pricing, insurance formularies, and even doctor habits can get in the way.
And then there’s the bigger picture: medication safety, the quiet, daily act of making sure your drugs don’t harm you. Whether you’re on warfarin and worried about interactions with antibiotics, or managing insulin and beta-blockers that hide low blood sugar signs, the brand name doesn’t change the risk. What matters is knowing your drugs, reading labels, and asking questions. A brand-name label won’t warn you about photosensitivity or C. difficile risk any better than a generic one. The real protection comes from understanding how your meds work, tracking side effects, and knowing when to check in with your doctor.
You’ll find posts here that break down real cases—like why some people’s INR spikes on Bactrim, how energy drinks clash with Adderall, or how thyroid meds can go wrong if misused. These aren’t theoretical warnings. They’re lived experiences. And they all tie back to one truth: whether you’re taking a brand-name or generic drug, your health doesn’t care about the label. It cares about what’s inside, how you take it, and whether you’re paying attention.
Generic Drugs vs. Brand-Name Medications: What You Really Need to Know
Generic drugs save up to 85% on prescription costs and work just as well as brand-name meds for most people. Learn when they're safe, when to stick with the brand, and how to avoid hidden risks.