COPD treatment: clear, practical steps you can take today
Got COPD and feeling overwhelmed by options? You’re not alone. COPD treatment aims to reduce symptoms, prevent flare-ups, and keep you active. Below are simple, proven steps and real-world tips to help you manage breathing problems better.
Medications and inhalers that actually help
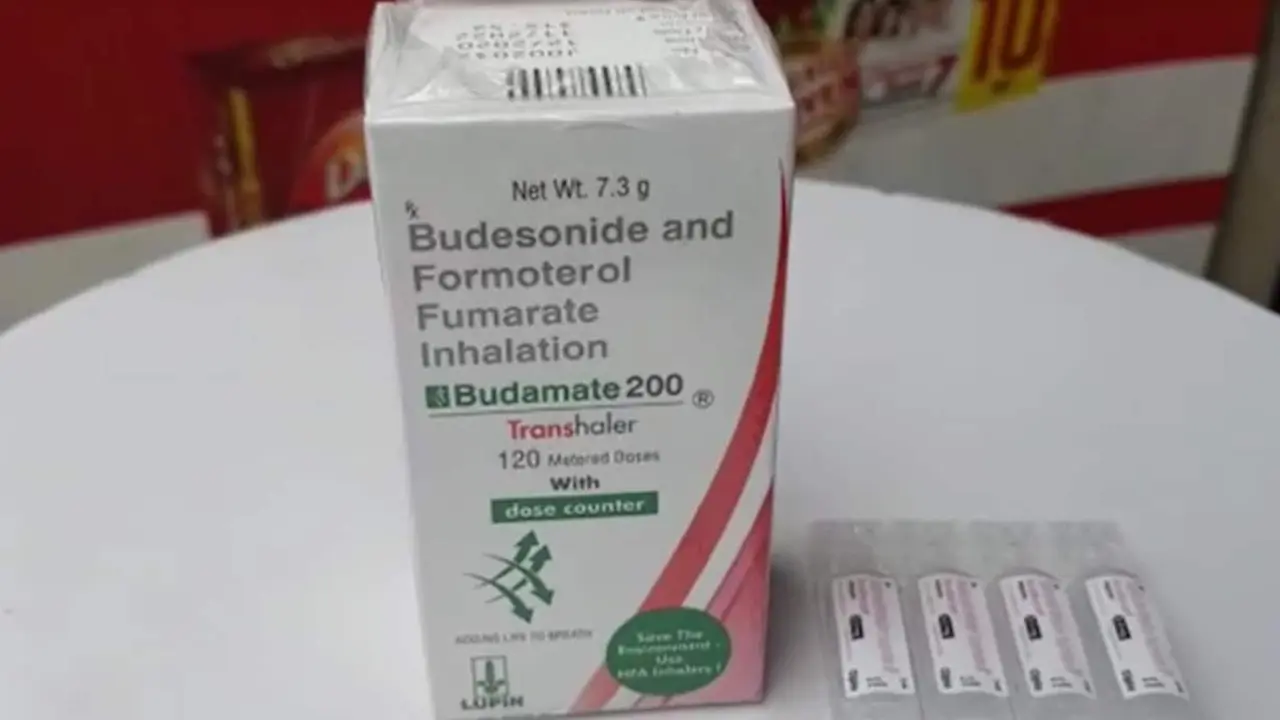
Most people with COPD use inhalers. There are a few main types: short-acting bronchodilators (rescue inhalers like salbutamol/Ventolin), long-acting bronchodilators (LABA and LAMA), and inhaled corticosteroids (ICS). Many patients do best on a combination inhaler—LABA + LAMA, or LABA + ICS. Triple therapy (LABA + LAMA + ICS) is an option if symptoms and flare-ups continue despite other meds. Newer single-inhaler triple options like Trelegy are on many lists for 2025; ask your doctor if that fits you.
Oral meds can help too. For frequent exacerbations with chronic bronchitis, doctors sometimes prescribe roflumilast. Mucolytics and short courses of antibiotics or steroids may be used during flare-ups. Always follow your prescriber's directions and ask about side effects.
Daily habits and rehab that make a real difference
Quit smoking. No single change beats this one for slowing COPD progression. If you need help, talk to your doctor about nicotine replacement, medications, or counseling—combining treatments works best.
Pulmonary rehab is often underrated. It’s a supervised program of exercise, breathing training, and education. People who finish rehab breathe easier, walk farther, and feel less anxious. If you can join even a short program, it’s worth it.
Learn proper inhaler technique. A poorly used inhaler is like an unused one. Ask a nurse or pharmacist to check your form—spacers and training devices can help. Keep a rescue inhaler handy and know your personal action plan for flare-ups: when to use rescue meds, when to start steroids or antibiotics if prescribed, and when to call for help.
Vaccines matter. Get your annual flu shot and a pneumococcal vaccine if advised. Infections often trigger severe flare-ups.
Other practical tips: stay active with paced walking or cycling, eat balanced meals to keep strength up, manage weight, and avoid smoky or dusty environments. If breathlessness is severe, home oxygen or a referral to a specialist for surgery or transplant assessment might be discussed.
Watch for warning signs: increased cough, change in mucus color, more breathlessness, fever, or swelling in legs. Those mean call your care team quickly.
Finally, keep talking with your healthcare team. Ask about newer inhalers, side effects, and how often to review your plan. Small changes—better inhaler use, rehab, vaccines, and quitting smoking—add up fast. You can make breathing easier and stay active longer.
Asthma vs. COPD: Key Differences in Symptoms and Treatment
Asthma and COPD both cause breathing trouble, but they're very different. Learn how symptoms, causes, and treatments differ - and why getting the right diagnosis matters.
Symbicort Prescription Online: A Comprehensive Guide to Managing Asthma and COPD
This detailed article explores the nuances of getting a Symbicort prescription online, its medical and side effects, and drug interactions with Budesonide and Formoterol substances. Readers will find in-depth analysis of the most common dosages and recommendations for using this medication to manage asthma and Chronic Obstructive Pulmonary Disease (COPD). Learn how to navigate the complexities of online prescriptions and ensure proper use to maximize benefits and minimize risks.