Safe combination: Practical guide to mixing medicines, alcohol and supplements
Mixing medicines, alcohol, or supplements without checking first can cause side effects, reduce treatment effectiveness, or create dangerous interactions.
This page pulls together clear, useful tips so you can make safer choices fast.
How to check if a combination is safe
First, read labels and leaflets. Manufacturers list major interactions and warnings right on the box or patient leaflet.
Second, use reputable online interaction checkers from national health services or verified pharmacies. Enter both prescription and over-the-counter items, including vitamins and herbal products.
Third, ask a pharmacist. They see these questions every day and can flag serious risks like bleeding, heart rhythm changes, or dangerous blood pressure drops.
Common risky combinations to watch for
Mixing alcohol with sedatives or strong painkillers often causes excessive drowsiness, breathing problems, and falls. If you take benzodiazepines, opioids, or certain sleep aids, avoid alcohol.
Combining blood thinners like warfarin with NSAIDs, some antibiotics, or high doses of vitamin K can increase bleeding risk or change drug levels. Check with your clinic before adding new meds.
Antidepressants mixed with certain pain medicines, migraine drugs, or supplements such as St John's Wort can cause serotonin syndrome — a potentially serious reaction with agitation, fever, and rapid heartbeat.
Potassium-sparing drugs like spironolactone plus potassium supplements or salt substitutes can raise potassium too high and harm the heart. Monitor levels if your doctor recommends combined use.
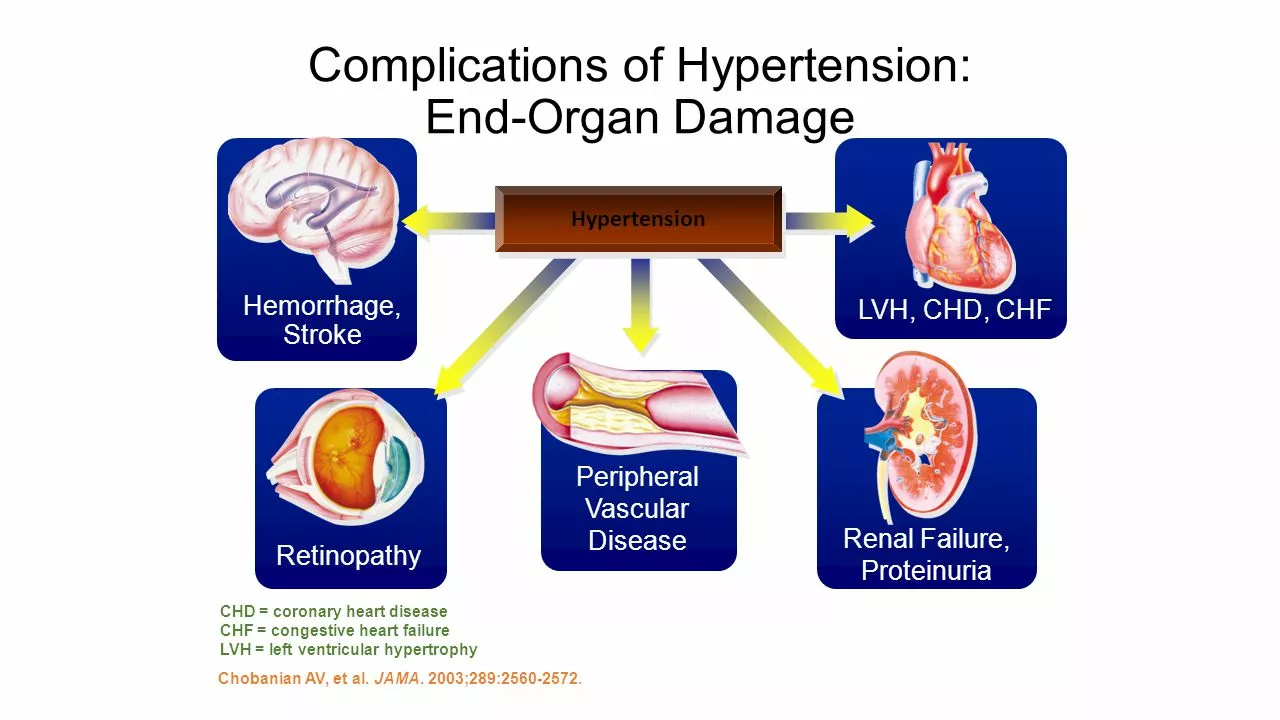
Some OTC cold medicines contain decongestants that raise blood pressure and interact with heart meds. If you have heart disease or take blood pressure pills, read ingredient lists or ask a pharmacist.
If you use inhalers or asthma medications and compete in sport, check WADA rules and your prescription paperwork before travel or competition.
Always tell every clinician and pharmacist about all substances you use — prescribed meds, supplements, recreational drugs, and frequent alcohol use. Small details matter, like allergy history or a past bad reaction.
Keep a current list of medicines on your phone. Include doses, how often you take them, and the prescribing doctor. Share that list at every medical visit and upload it to any patient portal you use.
If you see worrying symptoms after combining substances — fainting, severe dizziness, breathing trouble, chest pain, heavy bleeding, sudden confusion, or high fever — get emergency help right away.
When in doubt, pause new supplements and ask a professional. Online pharmacies and reviews can help find sources, but safety checks and prescriptions should come from qualified clinicians and accredited pharmacies.
Before travel, carry medicines in original packaging, pack a copy of prescriptions, and check legal status of controlled drugs in destination countries. Use pharmacy verification tools and read recent user reviews when ordering online. If cost is an issue, ask your prescriber about generic options or patient assistance programs. Small actions like setting phone reminders for doses and checking expiry dates prevent errors. Regular medication reviews with your doctor catch changing needs and reduce risky combinations over time.
Stay safe.
How to Safely Combine Azilsartan with Lifestyle Changes for Hypertension Management
Managing hypertension can be a bit of a challenge, but with the right approach, it's definitely doable. I've discovered that combining the use of Azilsartan with certain lifestyle changes can make a huge difference. It's all about maintaining a healthy diet, regular physical activity, and minimizing stress. However, it's crucial to take Azilsartan under medical supervision as it can have side effects. Remember, consistency is key and it's about balancing medication with lifestyle adjustments in a safe manner.