Antidepressants During Pregnancy
When you're pregnant and struggling with depression, the question isn't just antidepressants during pregnancy—it's what happens if you don't take them. Depression during pregnancy isn't just sadness. It’s exhaustion that doesn’t go away, panic attacks at 3 a.m., or feeling like you’re failing before your baby is even born. And yes, treating it matters—for your health, your baby’s development, and your ability to bond after birth. Antidepressants during pregnancy, medications like SSRIs and SNRIs used to treat depression in expectant mothers. Also known as prenatal antidepressants, these drugs cross the placenta and reach the fetus, which is why choices here aren’t simple. The real issue isn’t whether they’re safe or dangerous—it’s whether the risks of untreated depression are worse.
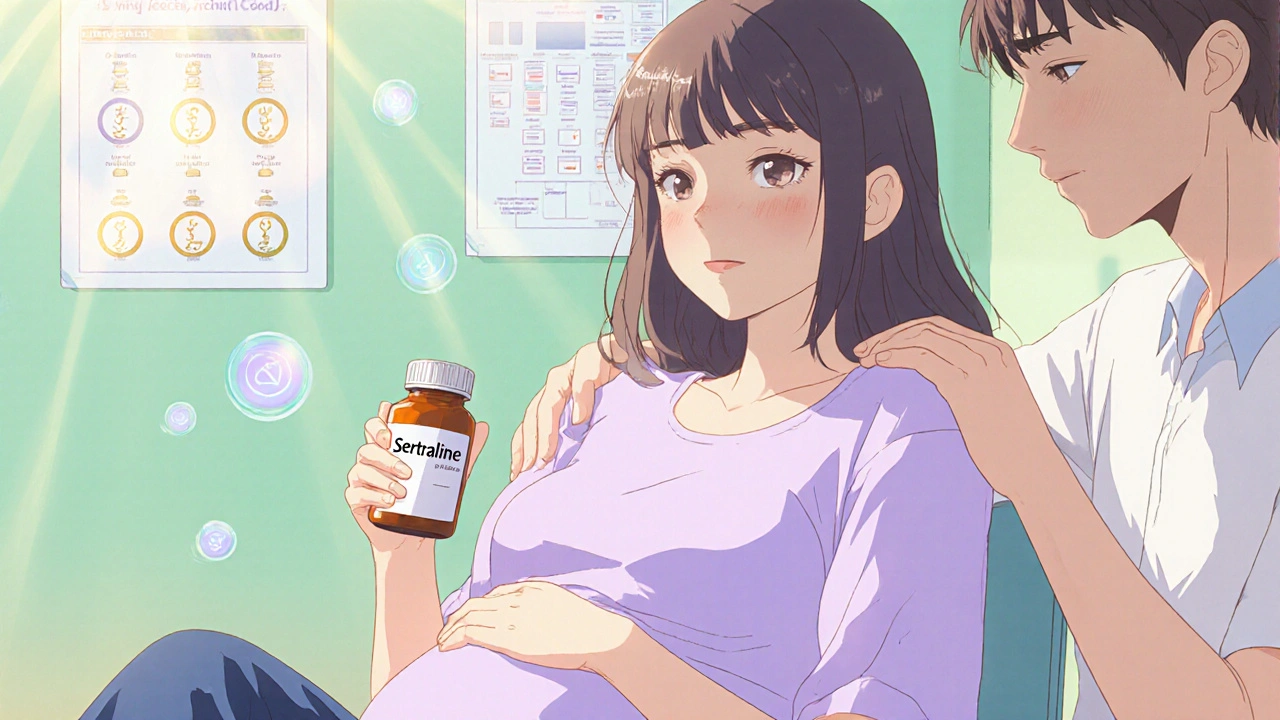
SSRI pregnancy, the use of selective serotonin reuptake inhibitors like sertraline or fluoxetine during gestation is the most studied area. Research from the New England Journal of Medicine and the American College of Obstetricians and Gynecologists shows that while some babies exposed to SSRIs may have slightly higher risks of temporary breathing issues or jitteriness at birth, these effects usually fade within days. Meanwhile, women who stop their meds often see depression return—sometimes severely—increasing the chance of preterm birth, low birth weight, or even postpartum suicide. Prenatal depression, a clinical mood disorder affecting up to 1 in 7 pregnant women isn’t something you can outwillpower. It’s a biological condition, just like high blood pressure or gestational diabetes. And just like those, it sometimes needs medical treatment.
There’s no one-size-fits-all answer. Some women switch to sertraline, which has the most safety data. Others taper off under supervision. A few combine therapy with low-dose meds. What’s clear from real-world data? Women who work with their OB and psychiatrist to make a plan have better outcomes than those who go it alone or quit cold turkey. Medication safety, the balance between drug risks and the dangers of leaving mental illness untreated is the core of every decision. And fetal development, how a baby’s brain and organs grow in response to chemicals in the womb isn’t just about drugs—it’s about stress hormones, sleep, nutrition, and whether you feel supported.
What you’ll find below aren’t abstract studies or scare tactics. These are real, practical posts from people who’ve walked this path—how to spot warning signs of withdrawal in newborns, what to ask your doctor before your next appointment, how to weigh the risks of untreated anxiety against the risks of meds, and why some women choose to go off antidepressants while others don’t. No fluff. No judgment. Just facts, stories, and tools to help you make the right call—for you, and your baby.
Antidepressant Use in Pregnancy: What You Need to Know About Safety and Side Effects
Antidepressants during pregnancy are safer than many think. Sertraline is the preferred choice, with no proven link to birth defects or long-term harm. Untreated depression poses greater risks to mother and baby.