Plaque psoriasis — what it looks like and how to manage it
Plaque psoriasis is the most common form of psoriasis. You’ll see raised, red patches covered with silvery scales, usually on the elbows, knees, scalp or lower back. It can itch, burn or crack, and severity ranges from small spots to large areas that affect daily life.
Treatment options that actually help
Topical treatments are the first step for mild to moderate plaque psoriasis. Corticosteroid creams, vitamin D analogues and moisturizers reduce redness and scaling. Use them as your dermatologist directs — too much steroid can thin skin, so cycles and correct application matter.
Phototherapy (narrowband UVB) helps when creams aren’t enough. It reduces immune activity in the skin and often clears stubborn patches after a few weeks. Clinics monitor dosing to lower long-term risks.
For moderate to severe cases, oral or injected systemic drugs work better. Methotrexate, cyclosporine and newer biologics target the immune signals that drive psoriasis. Biologics (like TNF or IL inhibitors) can give long-lasting control but require doctors to check infections and vaccinations first.
Daily care, triggers and simple habits that cut flares
Keep skin moist. Thick, fragrance-free emollients reduce scaling and stop cracks that invite infection. Apply them right after bathing to lock in water.
Watch triggers: stress, heavy alcohol, smoking, certain infections and some medications can spark flares. If you notice patterns — a flare after a cold, or worse with alcohol — tell your clinician and try changing that habit step-by-step.
Small lifestyle moves add up. Warm (not hot) baths with mild cleansers, gentle exfoliation of loose scales, and avoiding harsh soaps help. Maintain healthy weight and regular exercise — losing even a little weight can improve response to treatment.
When starting or changing meds, ask your doctor about realistic timelines: topicals might show results in weeks, phototherapy in a month or two, and biologics sometimes need several months for full effect. Also ask about side effects, monitoring tests, and vaccine needs.
Mental health matters. Psoriasis affects how you feel and how others see you. If anxiety or low mood shows up, talk to your doctor. Support groups and practical counseling often help more than people expect.
If patches are painful, spreading quickly, affecting joints (joint pain or swelling), or interfering with sleep or work, see a dermatologist fast. Early treatment cuts long-term damage and gives more options.
Use this tag page to explore articles, reviews and practical tips on treatments and lifestyle changes. If you’re trying new treatments, keep notes on what helps and what doesn’t — that record makes appointments far more productive.
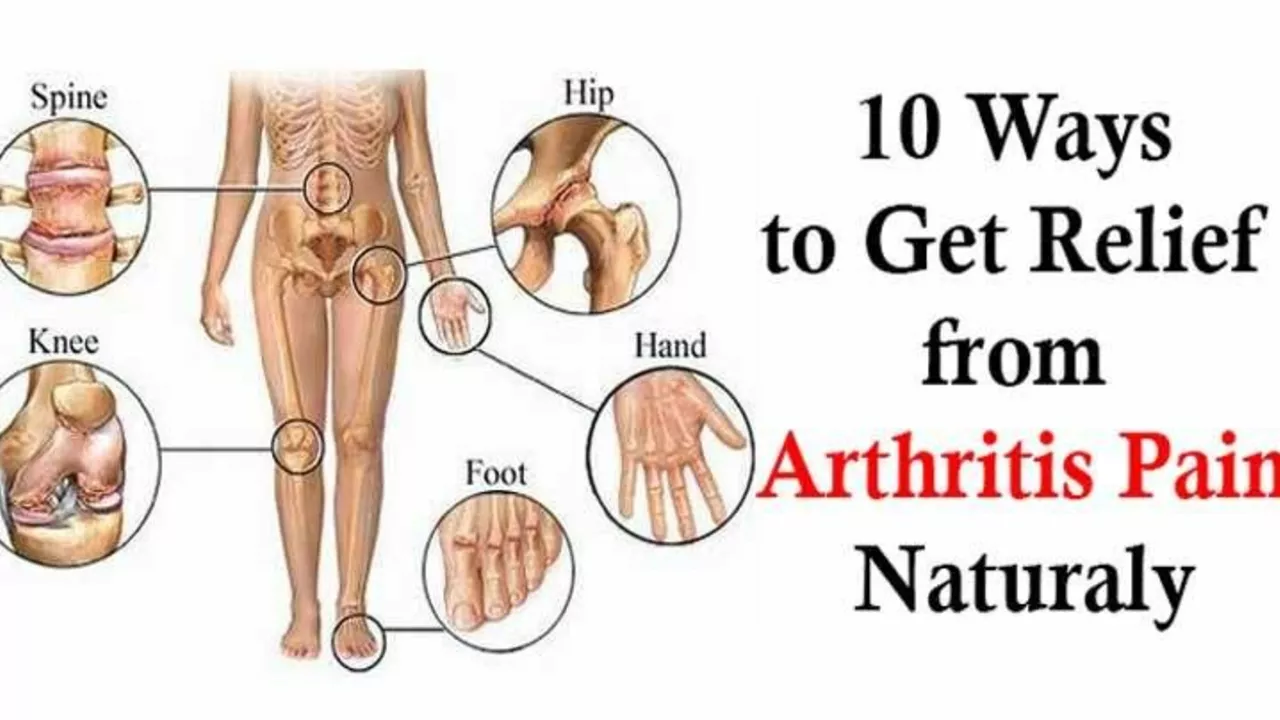
The Connection between Plaque Psoriasis and Joint Pain
In my recent exploration, I've discovered a fascinating link between plaque psoriasis and joint pain. It turns out, nearly 30% of people with plaque psoriasis also develop a condition known as psoriatic arthritis, which is characterized by joint pain. Moreover, psoriasis inflammation doesn't just affect the skin but can also impact the joints leading to discomfort and pain. It's critical to consult with a healthcare professional if you're experiencing joint pain along with psoriasis, as early diagnosis and treatment can help manage the symptoms. This connection emphasizes the complexity of psoriasis and its impact beyond skin symptoms.