Psoriatic Arthritis Treatment: What Works, What to Avoid, and How to Stay in Control
When psoriatic arthritis, a type of inflammatory arthritis that affects people with psoriasis, causing joint pain, swelling, and stiffness. Also known as PsA, it doesn’t just hurt—it can permanently damage joints if left unchecked. Many assume it’s just a skin issue that happens to flare up in the joints. But psoriatic arthritis is its own disease, with unique triggers, progression patterns, and treatment needs that set it apart from regular rheumatoid arthritis or osteoarthritis.
Effective DMARDs, disease-modifying antirheumatic drugs that slow or stop joint damage in inflammatory arthritis like methotrexate or sulfasalazine are often the first line of defense. But if those don’t cut it, biologic drugs, targeted therapies that block specific parts of the immune system driving inflammation like adalimumab, ustekinumab, or secukinumab can make a huge difference. These aren’t magic pills—they come with risks, require monitoring, and don’t work for everyone. But for many, they’re the only thing that stops the pain from getting worse.
What most people don’t realize is that treatment isn’t just about pills. Lifestyle changes matter—weight loss reduces pressure on joints, quitting smoking improves drug response, and gentle movement like swimming or yoga keeps stiffness at bay. And while some try to manage with OTC painkillers alone, that’s like putting a bandage on a broken bone. NSAIDs help with symptoms, but they don’t stop the damage underneath. That’s why monitoring matters: regular check-ins with your doctor, tracking joint swelling, and knowing when a drug stops working are just as important as the prescription itself.
There’s no one-size-fits-all plan. What works for your neighbor might do nothing for you. Some people respond to a single DMARD. Others need a combo. A few find relief with newer oral drugs like apremilast, which avoids injections but can cause nausea. And if you’ve been told your arthritis is "just mild," don’t accept that without proof. Joint damage can happen fast—even before you feel severe pain.
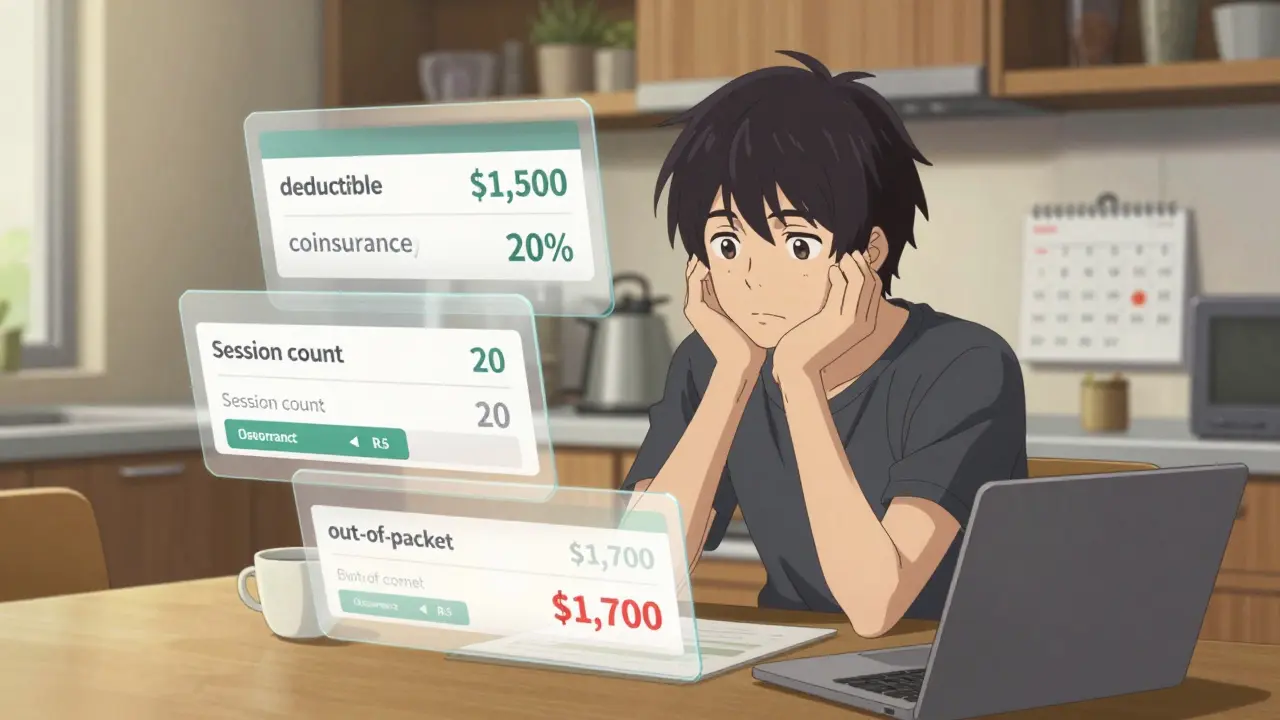
This collection brings together real, practical advice from people who’ve been there. You’ll find posts on how to spot early signs of joint damage, why some biologics work better than others, what to do when your insurance denies coverage, and how to handle side effects without quitting treatment. There’s no fluff here—just clear, no-nonsense info on what actually helps, what to watch out for, and how to keep your joints moving longer.
Psoriatic Arthritis: How Skin Disease Turns Into Joint Pain
Psoriatic arthritis links skin psoriasis with joint pain, swelling, and stiffness. Learn how it differs from other arthritis types, why early diagnosis matters, and what treatments actually work.